Last Updated on 19 September, 2025
Rule status: Proposed. Last checked [19 September, 2025]. See docket.
We monitor the Federal Register docket and will update this blog post when a final rule is published.
Sleep apnea is one of the most commonly claimed disabilities among veterans, and in 2025, the Department of Veterans Affairs (VA) proposed significant changes to the way it rates this condition. Many veterans rely on their VA disability ratings for financial support, and these changes may impact future claims.
Below, we will break down the current rating system, explain the proposed VA sleep apnea rating changes for 2025, and provide guidance, as noted by accredited VA attorney Rebecca Deming of ProVet Legal, on how veterans can protect their benefits.

Table of Contents
What is Sleep Apnea in Veterans?
Sleep apnea is a serious sleep disorder in which breathing repeatedly stops and starts during sleep. It is a prevalent condition among veterans, often linked to PTSD, traumatic brain injuries, facial or neck injuries, and prolonged exposure to smoke, burn pits, dust, and chemical agents during service. These risk factors can damage the respiratory system and disrupt the brain’s ability to regulate breathing.
There are three main types, namely,
- Obstructive Sleep Apnea (OSA)
- Central Sleep Apnea (CSA)
- Complex Sleep Apnea
Common sleep apnea symptoms include loud snoring, choking or gasping for air, excessive daytime sleepiness, and difficulty concentrating. If untreated, sleep apnea can lead to complications like high blood pressure, heart disease, diabetes, atrial fibrillation, and even death due to low blood oxygen.
A study published in the American Journal of Health Promotion found that obstructive sleep apnea (OSA) was diagnosed in 21% of veterans, more than double the 9% prevalence observed in nonveterans.
Veterans diagnosed with sleep apnea may also be eligible for VA disability benefits if the condition is connected to their military service.
Key Requirements for Service Connection
To qualify for VA disability benefits for sleep apnea, a veteran must generally show three things:
- A Current Medical Diagnosis
A VA-recognized sleep study (polysomnography) confirming obstructive, central, or complex sleep apnea.
- An In-Service Event, Injury, or Exposure
Evidence from service records, deployment history, or lay/buddy statements showing incidents or conditions during military service that could have caused or aggravated the sleep apnea (for example, hazardous exposure, facial injuries, or medications linked to weight gain).
- A Nexus Linking the Two
A medical opinion stating that it is “at least as likely as not” that the diagnosed sleep apnea is related to military service or to an already service-connected disability.
Without all three elements, VA may deny the claim or assign a lower rating. Including secondary service-connection evidence (we’ll explore them later in this blog) can also strengthen your case.
Current VA Sleep Apnea Disability Ratings
Under the current system, the VA rates sleep apnea under Diagnostic Code 6847 (38 C.F.R. § 4.97) at 0%, 30%, 50%, or 100% depending on the severity of symptoms and required treatment. Here’s the full rating criteria:
- 0% Rating: A veteran has a diagnosed condition but does not experience significant symptoms or require treatment. No monthly compensation for the rating itself.
- 30% Rating: The veteran has persistent daytime hypersomnolence (excessive sleepiness during the day). This rating qualifies for a monthly VA payment of about $537.42.
- 50% Rating: The veteran requires a CPAP (Continuous Positive Airway Pressure) machine or another breathing assistance device. A 50% rating warrants monthly compensation of roughly $1,102.04.
- 100% Rating: The veteran has chronic respiratory failure, requires around-the-clock oxygen, or has undergone a tracheostomy. As a result, the veteran receives full monthly compensation of approximately $3,831.30.
*Rates assume a single veteran with no dependents; amounts may increase with dependents. View official disability pay rates here.
The 50% rating is the most common because many veterans receive a CPAP prescription. However, the VA has proposed changes to this rule in 2025.
Why Is the VA Changing Sleep Apnea Ratings?
The VA first proposed overhauling its respiratory ratings, including sleep apnea, in a Notice of Proposed Rulemaking published on February 15, 2022 (87 FR 8474). After reviewing public comments, the agency issued a Supplemental Notice of Proposed Rulemaking on September 12, 2024, with revised criteria (89 FR 74162). These changes are still proposed; no final rule or effective date has been issued. Until a final rule is published in the Federal Register, sleep apnea continues to be rated under 38 C.F.R. § 4.97, Diagnostic Code 6847.
According to the VA, these changes are part of an ongoing effort to modernize the Schedule for Rating Disabilities and align evaluations with current medical understanding (VA News, 2024).
Top Reasons Behind the Overhaul
After years of mounting pressure from lawmakers, medical professionals, watchdog groups, and veterans’ advocates, the Department of Veterans Affairs is proposing changes to its sleep apnea rating system for these reasons:
- Automatic CPAP VA Rating: Under the current rating system, a prescription for a CPAP machine automatically grants a 50% VA disability rating, regardless of whether the device is used regularly or if symptoms improve significantly.
- Treatment Over Impact: The existing approach drew criticism for increasing disability ratings solely on treatment equipment, not the actual functional impairment a veteran experiences.
- Fairer Medical Assessment: Under the old VA rating system, veterans with well-managed symptoms received the same ratings as those with severe, treatment-resistant sleep apnea. The new sleep apnea VA rating offers a fairer assessment by factoring in treatment effectiveness, comorbidities and end-organ damage to accurately reflect functional impairment.
- Reduce Overcompensation: The VA seeks to limit high disability compensation for sleep apnea claims based mainly on CPAP prescriptions, especially when treatment is effective and symptoms are minimal.
Hence, advancements in the treatment and management of sleep apnea have prompted the VA to revise its rating criteria. However, many veteran advocacy groups argue that these anticipated changes unfairly penalize veterans who rely on CPAP therapy, as it fails to acknowledge that the lifelong use of the device is itself a burden.
While well-intentioned, these rules could also mean reduced compensation for veterans who don’t act before the proposed VA sleep apnea rating changes are implemented on the Federal Register effective date.
Major Proposed Changes to VA Sleep Apnea Ratings in 2025
One of the most significant proposed changes in the VA sleep apnea rating system is that a CPAP machine alone will no longer guarantee a 50% disability rating. This means the elimination of a 30% rating. Instead, the VA will assess sleep apnea based on how effective treatment is and the level of impairment experienced by the veteran.
New Sleep Apnea Ratings in 2025 (Proposed)
- 0% Rating: The veteran is asymptomatic with or without treatment.
- 10% Rating: The veteran has sleep apnea but experiences incomplete relief from symptoms despite treatment, as determined by a sleep study.
- 50% Rating: The veteran has ineffective treatment (as found in a sleep study) or is unable to use prescribed treatment due to comorbid conditions, and without end-organ damage.
- 100% Rating: The veteran has ineffective or unusable treatment due to comorbid conditions and suffers from end-organ damage (significant damage to major organs like the heart, lungs, kidneys, or eyes caused by sleep apnea).
If the sleep apnea VA rating changes are published, the VA will apply the new criteria to future claims. Until then, current ratings remain under 38 CFR §4.97 (Diagnostic Code 6847).
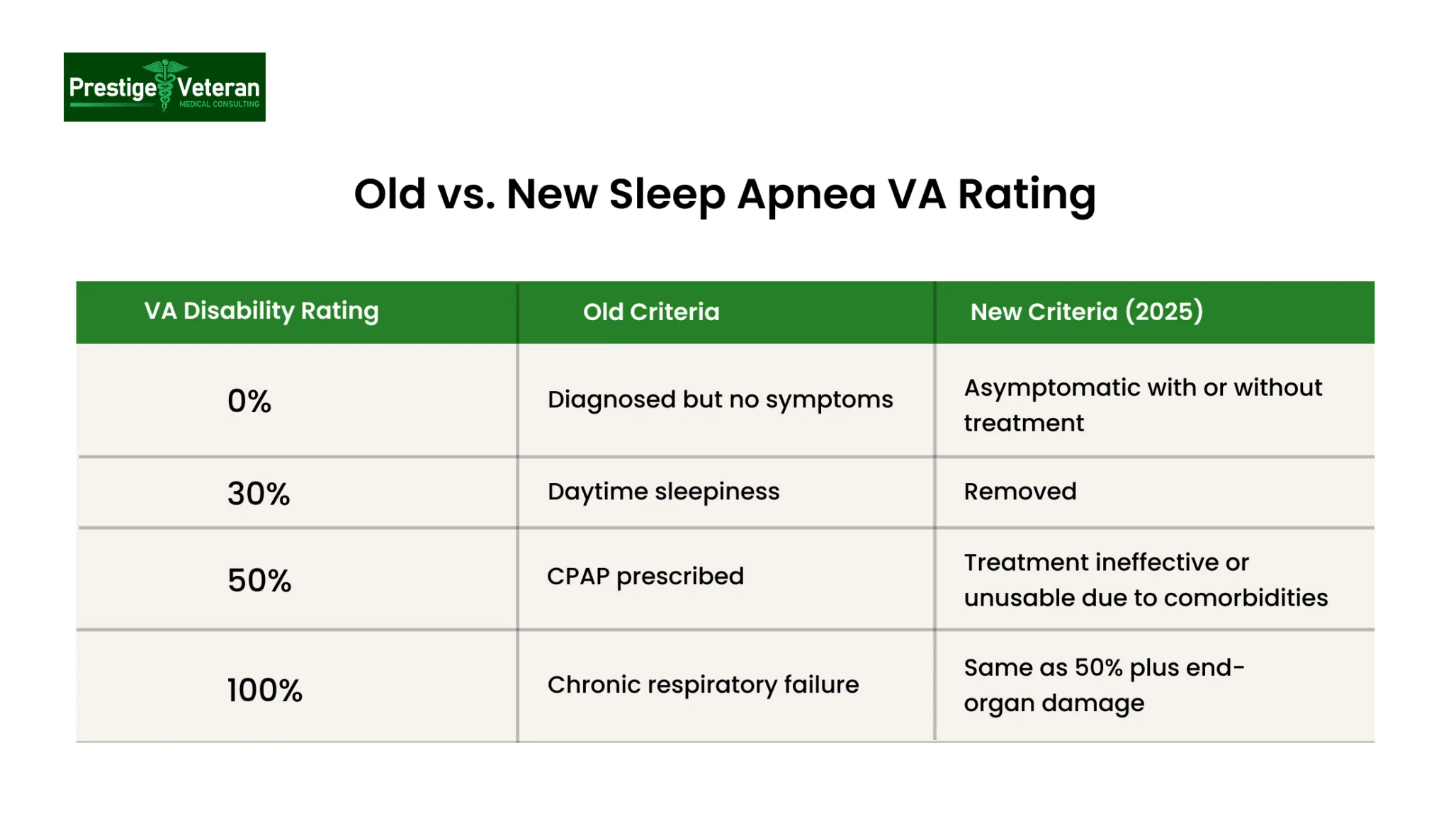
Current vs. Proposed VA Sleep Apnea Ratings
|
VA Disability Rating |
Current Rules (38 CFR §4.97 – DC 6847) |
*Proposed Rules (2025 – if finalized as proposed) |
|
0% |
Diagnosed, but no symptoms |
Asymptomatic with or without treatment |
|
30% |
Persistent daytime hypersomnolence |
Removed |
|
50% |
Requires CPAP or other breathing assistance |
Treatment is ineffective or unusable due to comorbidities |
|
100% |
Chronic respiratory failure, tracheostomy, or oxygen 24/7 |
Treatment is ineffective or unusable due to comorbidities, plus end-organ damage |
(These are PROPOSED changes. Current ratings remain under 38 CFR §4.97 (DC 6847) until a FINAL rule is effective.)
VA’s Proposed Rule on Comorbid Conditions
In 2022, VA proposed revising DC 6847 to consider comorbid conditions when rating a veteran’s sleep apnea. These comorbidities can make standard sleep apnea treatments like CPAP machines ineffective or unusable and can also lead to end-organ damage.
Under that proposed rule (not yet in effect), the VA will take comorbid conditions into account, particularly when determining eligibility for a 50% or 100% rating.
What are the Comorbid Conditions for VA Sleep Apnea?
In the proposed rule, VA plans to add an informational note defining and giving examples of qualifying comorbid conditions as those that, according to a qualified medical provider, directly impede or prevent the use or implementation of a recognized treatment intervention that is normally considered effective.
The listed examples are contact dermatitis at the mask site, Parkinson’s disease, facial disfigurement, missing limbs, or skull fracture, conditions that directly interfere with sleep apnea treatment.
See 87 Fed. Reg. 8474 (Feb. 15, 2022).
Why Comorbidities Still Matter
Even under the current criteria (38 C.F.R. § 4.97, DC 6847), comorbid conditions can indirectly affect a VA claim for sleep apnea:
- They can appear in medical evidence showing the overall severity of a veteran’s health picture.
- They can support secondary service-connection claims (for example, sleep apnea caused or aggravated by another service-connected condition).
- They may help establish why a veteran cannot tolerate or use a prescribed device, which could become relevant if VA finalizes its proposed rule.
Proving a Comorbid Condition for a Higher Rating
In recent years, manufacturers have estimated that around 8 million people across the United States rely on CPAP machines. To secure a 50% or 100% rating, veterans should consider providing:
- Medical evidence of a secondary comorbid condition (doctor’s diagnosis, treatment records).
- A nexus letter linking the comorbid condition to sleep apnea or military service. While never required, these can at times be helpful.
- Sleep studies showing that CPAP is ineffective or unusable.
If treatment is ineffective or unusable due to comorbidities and leads to organ damage, a veteran may qualify for a 100% disability rating.
How Will These Proposed Changes Impact Veterans?
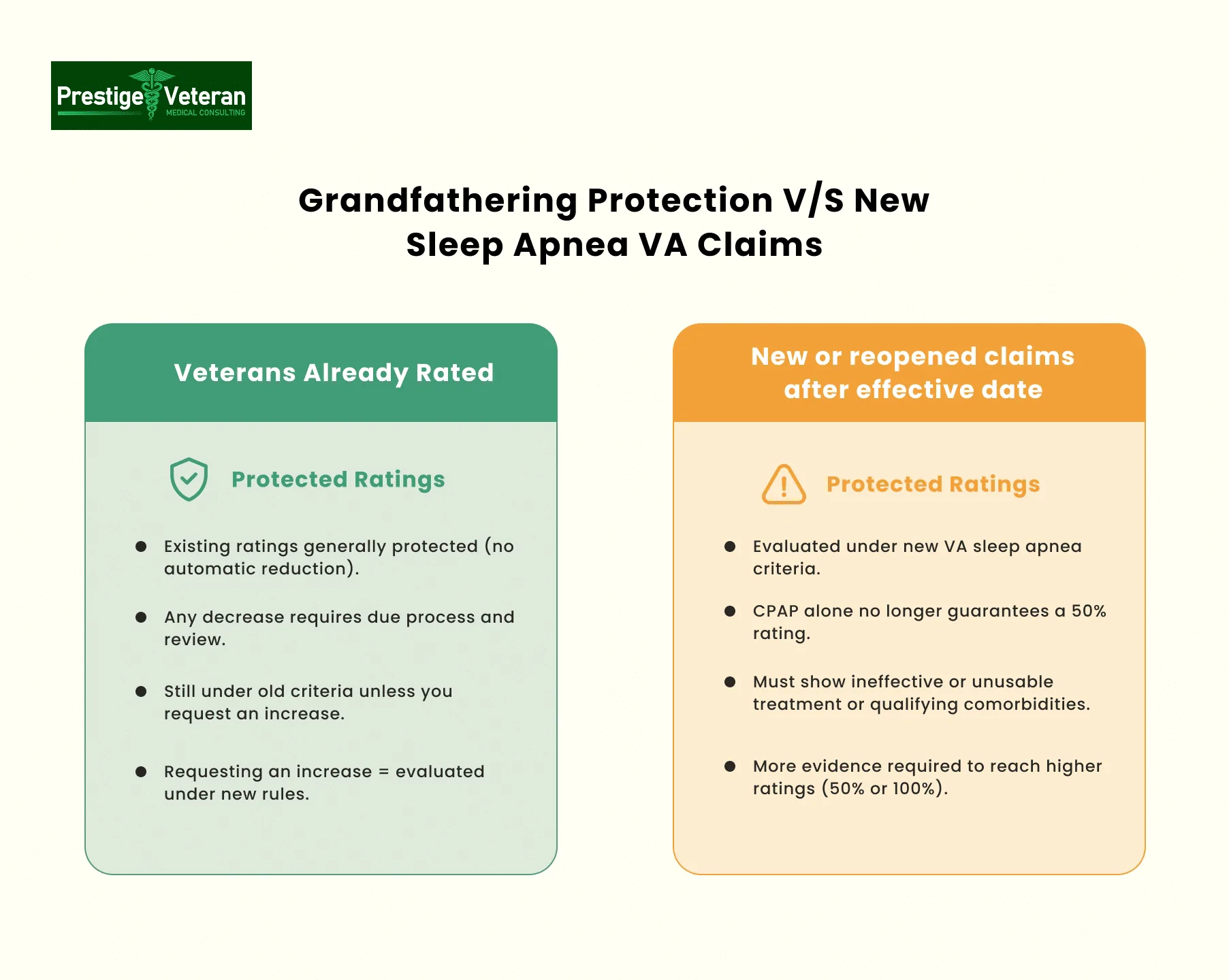
Veterans Already Receiving a Sleep Apnea Rating
If you already have a VA disability rating for sleep apnea, it will generally remain protected under “grandfathering” provisions. This means your existing rating will not be lowered automatically, as any reduction would require due process and compliance with protected-rating rules. However, if you later request an increased rating, the VA will evaluate your claim under the new criteria.
Veterans Filing New Claims
Veterans whose sleep apnea claims are filed or reopened after the rating change effective date will be evaluated under the new criteria. It is important to check with a legal professional for verification of the official date.
This means that simply receiving a CPAP prescription will not be enough to secure a 50% rating. Veterans will need additional medical evidence to demonstrate that their treatment is ineffective or that they cannot tolerate the prescribed treatment due to other comorbid conditions.
Veterans With Pending Claims
If your sleep apnea claim was filed before the rating change effective date but is still pending, VA will apply the rating criteria most favorable to you. The decision will consider both old and new and apply whichever is more favorable from the change date forward. (VAOPGCPREC 3-2000, §3.114)
Veterans Requesting an Increased Rating
If you are currently rated for sleep apnea and request an increase after the confirmed change date, your claim will be reviewed under the new criteria. While your existing rating is generally protected, it may be subject to reevaluation under due-process rules, which may lead to a proposed reduction if treatment is considered effective. This is why many legal experts advise veterans to be cautious when requesting increases.
How to Get VA Disability for Sleep Apnea?
Many veteran advocates like Ms. Deming recommend that if you suspect you have sleep apnea, file a claim before the new regulations take effect. Consulting with legal professionals is advised.
Submit an Intent to File (ITF) at VA.gov to lock in your effective date while you gather evidence. Filing early can help you qualify under the current, more favorable rating system and may maximize back pay.
To establish a service connection and maximize your chances of approval, follow these steps:
Step 1: Get a Recent Sleep Study & Diagnosis
Obtain a VA-recognized sleep study (polysomnography) within the last 12 months to confirm your diagnosis and current severity. It’s important to get an official medical diagnosis of sleep apnea from a sleep specialist before filing your VA claim.
Step 2: Identify In-Service Events or Conditions
Gather deployment records (DD-214), service treatment records, and personnel files showing exposure or incidents during active duty that may have caused or worsened your sleep apnea.
For instance, military environments, burn pits, weight gain linked to medications, or evidence of already service-connected disabilities.
Step 3: Obtain a Nexus Letter
A nexus letter from a qualified medical professional can link your sleep apnea to your service or another service-connected disability. It should state your condition is “at least as likely as not” related to service.
Step 4: Identify Secondary Service Connection
If your sleep apnea developed as a result of an already service-connected condition (for example, PTSD, weight gain, or deviated septum from service injury), file it as secondary to that condition. Clearly state this on your claim to strengthen your case.
Step 5: Gather Supporting Evidence
To strengthen your claim, collect:
- VA and private treatment records
- CPAP or BiPAP compliance data
- Buddy or lay statements describing in-service sleep issues or snoring symptoms
- If available, a completed DBQ for Sleep Apnea signed by your treating or VA provider
Step 6: Fill Out VA Form 21-526EZ
To file a sleep apnea VA claim, start by completing VA Form 21-526EZ, the Application for Disability Compensation and Related Compensation Benefits.
Download VA Form 21-526EZ (PDF)
Pay special attention to:
- Section V: Clearly list the conditions you’re claiming (e.g., “sleep apnea secondary to PTSD”). Add information on your military service history and the location of treatment facilities.
- Section VI: Include military service dates, branches, and duty locations, especially where symptoms began or exposures occurred that may have contributed to your sleep apnea.
Step 7: Submit the Form
You can file:
- Online at VA.gov
- By mail to the Evidence Intake Center
- In person through a Veterans Service Organization (VSO) or a VA-accredited attorney
You can check the status anytime at VA.gov/track-claims. Claims usually take 3–6 months, depending on complexity.
Step 8: Attend Your C&P Exam and Track Status
Most veterans will be scheduled for a Compensation & Pension (C&P) exam. Attend as scheduled and describe your symptoms honestly. You can also attach C&P exam results from prior claims to your VA disability application.
Filing before the new sleep apnea rating changes take effect may let you take advantage of the current automatic 50% rating for CPAP use.
Legal and Strategic Considerations
What If Your Claim Is in the Appeals Process?
If you filed a claim before the changes and your case is on appeal, you should still be evaluated under the old rating system. However, if your case was previously denied and you reopen it after the change date, the new criteria will apply.
Could These Changes Be Challenged?
Some veterans’ organizations have raised concerns about the fairness of these changes. While legal challenges are possible, the VA has already conducted a public comment period and moved forward with implementation. For now, veterans should assume the proposed changes may take effect in future as planned and act accordingly.
Sleep Apnea and Secondary Service Connection for VA Disability

The VA allows secondary service connection when medical evidence shows that another service-connected disability either caused or aggravated sleep apnea. Establishing this link can increase your overall VA rating and monthly compensation.
Below are key conditions often considered in secondary claims under 38 C.F.R. § 3.310:
- Rhinitis & Sinusitis: Chronic nasal inflammation can narrow airways, worsening or triggering obstructive sleep apnea. Medical records showing long-term ENT treatment can support a nexus opinion.
- Post-Traumatic Stress Disorder (PTSD): Veterans with PTSD may struggle with hyperarousal, disrupted sleep cycles, and medication side effects, which lead to weight gain and airway instability, aggravating sleep apnea. Moreover, PTSD and OSA share a bidirectional relationship.
- Depression & Anxiety – These mental health conditions, or their prescribed medications, may lead to weight gain and disrupted sleep, indirectly aggravating apnea. Stress-related claustrophobia can also prevent effective use of CPAP, potentially qualifying for a higher rating.
- Obesity (As an Intermediary Link: Weight gain related to service-connected conditions (like PTSD or medications) can be documented as the path between the primary disability and sleep apnea.
- Gastroesophageal Reflux Disease (GERD): Nighttime reflux due to GERD can irritate the throat and may interfere with comfortable breathing during sleep, making it harder for veterans to tolerate CPAP therapy.
- Asthma: Asthma may lead to ongoing airway inflammation and obstruction, heightening the risk of sleep-disordered breathing.
Tip: To strengthen your claim, obtain a medical nexus statement linking your primary service-connected condition(s) to secondary sleep apnea, include sleep study results, and document ongoing treatment.
Some related conditions, such as chronic rhinitis, sinusitis, and asthma, are now recognized on the VA’s presumptive list (effective August 5, 2021; see 86 Fed. Reg. 42,724). This means these respiratory conditions may qualify for presumptive service connection to sleep apnea if you served in specific locations during designated time frames.
Hence, giving combined evidence can significantly improve your chances of a favorable VA decision on secondary service connection.
Qualifying for TDIU with Sleep Apnea
Total Disability Individual Unemployability (TDIU) allows veterans whose service-connected sleep apnea prevents substantially gainful employment to receive compensation at the 100% disability rate even if their combined VA rating is below 100%.
Usually, veterans with OSA experience severe daytime fatigue, memory issues, cardiovascular issues, and impaired concentration, all of which can limit their ability to maintain gainful employment.
To qualify for TDIU under 38 C.F.R. § 4.16(a) (schedular), veterans generally need:
- A single disability rated at 60% or
- A combined rating of 70% with at least one condition rated 40%.
Veterans may also apply for extraschedular TDIU under § 4.16(b) if they don’t meet the percentage thresholds but cannot work.
Strong supporting evidence, such as medical opinions, employer statements, and lay testimony, may help demonstrate how your sleep apnea interferes with work. Veterans should clearly link their unemployability to their service-related disability by filing VA Form 21-8940 and ensure maximum benefits.
How Veterans Can Prepare for a VA C&P Exam for Sleep Apnea
A VA Compensation & Pension (C&P) exam for sleep apnea plays a pivotal role in determining a veteran’s eligibility for disability benefits. Conducted by a VA or contracted medical professional, this exam assesses three key factors: a confirmed diagnosis via sleep study, a nexus to military service, and the condition’s overall impact on life and functionality.
What to Expect:
- During the exam, the C&P examiner will review your full medical history, including prior sleep studies, treatments, and any use of breathing assistance devices like a CPAP machine.
- They may also evaluate secondary conditions like PTSD, obesity, or heart disease that aggravate sleep apnea.
- Expect questions about the onset and progression of symptoms such as loud snoring, gasping or choking during sleep, daytime hypersomnolence, or the need for a CPAP or BiPAP machine.
- Veterans will be asked how sleep apnea affects work, daily tasks, and social interactions.
- The examiner will complete a Sleep Apnea Disability Benefits Questionnaire (DBQ), which guides VA raters in deciding claims.
These findings directly influence the VA disability rating, which can range from 0% to 100% depending on functional impact.
How to Prepare:
Veterans should bring sleep study results, CPAP compliance and usage records to qualify for 30% or 50% VA rating, and written statements showing functional limitations.
When describing your symptoms, you can say, for example, “I’m constantly exhausted during the day and have trouble focusing at work due to poor sleep.”
Sometimes, the VA may conduct an ACE (records-only) review without an in-person evaluation. Regardless of format, being honest and detailed ensures the examiner can accurately capture the severity of your condition and strengthen the case for service connection.
The Essential Role of Nexus Letters in Sleep Apnea VA Claims
In VA sleep apnea, nexus letters are often a critical part of a successful claim, especially for veterans pursuing a 50% or 100% disability rating.
A nexus letter is an independent medical opinion written by a licensed physician or healthcare provider explaining how your sleep apnea is at least as likely as not caused or worsened by your military service or a service-connected condition.
An effective nexus letter for sleep apnea can include:
- Clear medical rationale using “at least as likely as not” language
- Explanation of why comorbid conditions make the treatment intolerable
- Documentation of End-Organ Damage, if applicable
- Reference to medical records, including sleep studies, treatment history, and documentation of symptoms
Veterans should aim to include nexus letters from VA or private doctors familiar with their medical history. While not legally required, these letters can be vital medical evidence for those filing claims under the updated rating criteria or appealing a denial.
Case Study: 50% VA Sleep Apnea Rating
A 38-year-old former Army veteran served on active duty from 2005 to 2013 with multiple deployments in high-stress environments. During service, his medical records documented chronic fatigue, difficulty staying awake during duty hours, and repeated complaints from roommates about loud snoring and pauses in breathing at night.
Following separation, his symptoms worsened, leading to morning headaches, impaired concentration, and elevated blood pressure. In 2024, a polysomnography confirmed a diagnosis of obstructive sleep apnea (OSA), and he was prescribed a continuous positive airway pressure (CPAP) machine.
Because his VA disability claim was filed before the proposed 2025 regulatory change, the claim is adjudicated under the current criteria. Under those rules, the use of a CPAP machine establishes eligibility for a 50% VA disability rating with corresponding monthly compensation.
Key Evidence Supporting the Claim:
- Service treatment records and witness statements showing in-service symptoms
- Post-service medical records documenting worsening of symptoms
- A 2024 polysomnography confirming OSA diagnosis and CPAP prescription
- A medical nexus opinion from a board-certified pulmonologist linking the veteran’s current OSA to documented in-service symptoms
- Evidence of secondary conditions (e.g., elevated blood pressure) supporting the impact and continuity of OSA
Nexus Statement:
“It is my professional medical opinion that it is at least as likely as not (a 50% probability or greater) that the veteran’s currently diagnosed obstructive sleep apnea (OSA) began during or is directly related to his active military service.”
(This example is for educational purposes only and does not constitute legal or medical advice.)
Authored by:
Rebecca Deming, Esq.
VA-Accredited Attorney, ProVet Legal
Specializing in VA disability law and military medical appeals
Medically Reviewed by:
Board-Certified Pulmonologist
VA Sleep Apnea Rating Changes in 2025 – Final Thoughts
The proposed 2025 changes to VA sleep apnea ratings will make it more difficult for veterans to receive a 50% disability rating. The key takeaway noted by Ms. Deming is that filing before the proposed changes are finalized is the best way to secure a favorable rating. If you believe you have sleep apnea, don’t delay—start gathering medical evidence and file your claim as soon as possible.
For veterans already rated for sleep apnea, the best approach is to avoid requesting an increase unless absolutely necessary, as doing so could put your rating at risk under the new system. If you have questions about your specific situation, consulting with a VA-accredited attorney or claims agent can help you navigate the process and protect your benefits.
FAQs
What is the effective date for the VA sleep apnea rating changes?
The Department of Veterans Affairs has proposed updates to its sleep apnea rating criteria, and if finalized, changes would come into force on the Federal Register effective date.
How can I obtain a higher VA rating for my sleep apnea?
To get a higher 50% VA rating under the proposed changes, you will have to submit medical evidence showing that CPAP is ineffective or unusable due to comorbid conditions. For a 100% rating, prove that the untreated sleep apnea causes end-organ damage.
Will the VA automatically decrease my current rating?
Generally, existing ratings are protected under “grandfathering” rules, but if you request an increase or VA re-evaluates your condition, it could propose a reduction following due-process requirements.
If I submit my claim now, but the VA doesn’t decide until after the sleep apnea changes effective date, which rules will be used?
If you file your disability claim before the new regulations take effect, it will be evaluated under the current, more favorable criteria, even if the VA issues a decision after the effective date.
Will using a CPAP machine still qualify for a 50% rating?
Under current rules, it does, but under the proposed 2025 changes, you will need to show that the CPAP treatment is ineffective or unusable due to comorbidities to qualify for 50%.
What’s considered “ineffective treatment”?
“Ineffective treatment” in VA sleep apnea claims refers to when prescribed CPAP therapy fails to control symptoms like daytime drowsiness, headaches, or difficulty concentrating, or improve the condition despite proper use, as verified by a sleep study.
What will justify a 100% rating for a sleep apnea VA claim?
To get a 100% VA rating for sleep apnea under the new rating system proposed by the VA, your treatment must be ineffective or unusable due to comorbidities, and you must have end-organ damage caused by the sleep apnea.
Will VA check CPAP compliance data?
Yes, under current rules, VA may review CPAP prescription and usage records, and under the proposed changes, ineffective or unusable treatment must be documented by a sleep study or medical evidence.
What counts as “end-organ damage”?
In the proposed criteria, end-organ damage means significant, medically documented harm to major organs such as the heart, lungs, kidneys, or eyes caused or aggravated by sleep apnea.
Do I need a new sleep study?
Yes, both current and proposed rules emphasize a recent, VA-recognized sleep study to confirm diagnosis, severity, and whether treatment is effective or unusable.
How does secondary to PTSD/GERD work?
You can file sleep apnea as secondary if medical evidence or a nexus letter shows it was caused or worsened by a service-connected condition, such as PTSD, GERD, or related weight gain.
Also read: The Role of a Nexus Letter for Obstructive Sleep Apnea (OSA) Claims
At Prestige Veteran Medical Consulting, a veteran-owned company, we specialize in Independent Medical Opinions (IMOs) known as Nexus letters.
Our purpose is to empower YOU, the veteran, to take charge of your medical evidence and provide you with valuable educational tools and research to guide you on your journey.
Understanding the unique challenges veterans face, our commitment lies in delivering exceptional service and support.
Leveraging an extensive network of licensed independent medical professionals, all well-versed in the medical professional aspects of the VA claims process, we review the necessary medical evidence to incorporate in our reports related to your VA Disability Claim.
Prestige Veteran Medical Consulting is not a law firm, accredited claims agent, or affiliated with the Veterans Administration or Veterans Services Organizations. However, we are happy to discuss your case with your accredited VA legal professional.















One Response
I was extremely short of breath and constantly tired due to my emphysema. I was advised to take Montair plus one tablet every night which would give me temporary relief and help my sleep. But I did not want to depend on the tablet fully, which only offers relief, not a cure. I slowly started Ayurveda and was introduced to LIMITLESS HERBS CENTER and their COPD Formula; my symptoms gradually diminished, including my shortness of breath, wheezing, and fatigue. Reach them at Limitless healthcenter . co m. I’m sharing this perhaps someone is also looking at genuine alternative treatment. I can vouch for these Ayurvedic treatments, but you still need to decide what works best for you. Sending prayers