Last Updated on 5 September, 2025
Obesity is a prevalent health concern that affects individuals across various demographics, including military veterans. In 2020, the obesity rate among veterans receiving care through the Veterans Affairs (VA) health system was 45.2%, significantly higher than the 42.4% national rate reported in 2018.
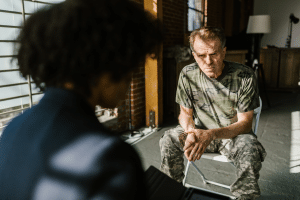
Leah Bucholz explains the intricate relationship between obesity and veterans’ disability, drawing insights from experiences and expertise.

Table of Contents
What Qualifies as Obesity for VA Disability?
Obesity is defined medically as having a Body Mass Index (BMI) of 30 or higher, which is calculated using a person’s height and weight. Although BMI doesn’t account for muscle mass or body composition, it remains the standard metric used by the Centers for Disease Control (CDC) and the Department of Veterans Affairs (VA). For instance:
- A 5’9” individual weighing 205 lbs would have a BMI just over 30.
- BMIs between 25 and 29.9 are considered overweight.
- A BMI of 40 or higher is classified as morbid obesity.
While obesity does not currently have its own VA diagnostic code, it may still serve as a critical factor in claims involving secondary service connection or TDIU (Total Disability based on Individual Unemployability). Understanding how obesity is defined is the first step toward building a strong claim.
Is Obesity a VA Disability? Understanding the Legal Landscape
In VAOPGCPREC 1-2017, the VA Office of General Counsel memo held that obesity is neither a “disease” nor a “disability” for direct service connection, so it does not get its own rating under the VA Schedule for Rating Disabilities (VASRD). Obesity by itself is not a VA-rateable disability, but it can still be key to winning service connection for other conditions and potentially lead to VA disability compensation.
Intermediate Step Theory
Under 38 C.F.R. § 3.310, if a service-connected condition causes or aggravates obesity and that obesity then leads to another disability, then the VA can grant the resulting condition on a secondary basis. For example, in Walsh v. Wilkie (2020), the U.S. Court of Appeals for Veterans Claims showed how PTSD treatment with psychiatric medications could cause weight gain, leading to obesity, which then contributed to diabetes. In such cases, diabetes may be service-connected as secondary to PTSD, with obesity serving as the crucial intermediate link.
The VA’s official M21-1 Adjudication Manual also instructs raters to consider obesity as an “intermediate step” when reviewing a secondary service connection.
Functional Impairment of Earning Capacity
In Larson v. McDonough (2021), the Federal Circuit held the Veterans Court has jurisdiction to decide what counts as a §1110 ‘disability’, reaffirming Saunders that ‘disability’ means functional impairment of earning capacity, but it did not decide whether obesity is compensable, as the case was remanded. This means obesity, if shown to directly hinder a veteran’s ability to work, could potentially qualify as a compensable disability.
Extraschedular Ratings
While rare, obesity caused by a service-connected disability may justify an extraschedular rating under 38 C.F.R. §3.321(b)(1) if it creates unusual impairment not captured by rating criteria. For instance, if a veteran’s back condition, originally rated at 40% develops obesity that severely restricts work beyond schedular limits, the VA could grant an extraschedular increase, raising the back rating to 60%, not obesity itself.
While you can’t get service connected for obesity itself, it can still be a powerful factor in linking other conditions to service.
Obesity as an Intermediate Step in VA Claims
The legal and medical framework of the “intermediary step” allows obesity to function as a bridge between a primary service-connected injury or illness to resulting disabilities that would otherwise be unrecognized for compensation.
VA’s Three-Part Test for Obesity as an Intermediate Step:
To use obesity as an intermediate step, you must prove three things:
- Your service-connected condition caused your obesity.
- Your obesity was a substantial factor that contributed to a new disability (e.g., sleep apnea, diabetes).
- That secondary condition would not have occurred but for obesity.
With a strong medical nexus, this pathway can enable veterans to secure compensation for obesity-related conditions like sleep apnea, diabetes, heart disease, or hypertension.
7 Common Secondary Conditions Linked to Obesity
If you are already service-connected for a disability that impairs mobility, disrupts metabolism, or requires medications known to cause weight gain, you may later develop obesity as a secondary effect. In such cases, the VA may qualify you for additional VA disability ratings based on related conditions.
Here are common secondary conditions often linked to VA disability for obesity:
1. Sleep Apnea
Obstructive Sleep Apnea (OSA) is frequently linked to obesity in veterans, as excess fat around the neck and throat narrows airways during sleep. This restriction causes repeated breathing interruptions, daytime fatigue, and raises cardiovascular risks. Many veterans also develop obesity-induced OSA as a secondary effect of PTSD medications or limited mobility.
Under VA’s proposed revision to DC 6847 (Feb 15, 2022), ratings for sleep apnea would be 0%, 10%, 50%, or 100% (adding 10% and eliminating 30%) based on symptoms, treatment effectiveness, and end-organ damage. This is not final as of Sept 6, 2025.
Currently, VA rates sleep apnea at 0%, 30%, 50%, or 100%, depending on daytime sleepiness, CPAP use, or respiratory failure.
2. Type 2 Diabetes
Excess weight contributes to insulin resistance, making obesity a primary cause of Type 2 diabetes. Veterans are especially vulnerable when service-connected injuries or medications trigger weight gain. Diabetes may begin with mild symptoms but can progress to requiring insulin therapy, a restricted diet, or even hospitalization. Since diabetes often leads to neuropathy, vision loss, or kidney damage, veterans should track progression carefully. This makes obesity a disability in terms of its role in the development of chronic metabolic disease.
VA disability ratings for diabetes range from 10%, 20%, 40%, 60%, to 100%, depending on the severity and insulin use.
3. Hypertension (High Blood Pressure)
Obesity increases cardiovascular workload, forcing the heart to pump harder and raising blood pressure levels. Veterans who are unable to maintain a healthy body weight due to service-connected physical or mental limitations often develop hypertension as a secondary condition, especially when obesity restricts physical activity. If left untreated, hypertension increases the risk of stroke, heart attack, and kidney disease.
Hypertension is commonly rated from 10%, 20%, 40%, to 60%, depending on blood pressure readings and medication use.
4. Orthopedic & Musculoskeletal Disorders
Excessive weight places tremendous strain on the spine, knees, hips, and feet, aggravating injuries and degenerative conditions such as osteoarthritis. Veterans with service-connected musculoskeletal issues often experience mobility decline and pain intensify due to obesity. Additionally, weight gain often worsens recovery from surgeries and limits rehabilitation success, making VA claims stronger when linked to service-connected injuries.
For example, back pain qualifies for disability ratings from 10%, 20%, 40%, 50%, or higher based on the severity of limited motion and whether the spine is ankylosed (fused).
5. Heart Disease
Veterans with obesity are at higher risk for ischemic heart disease, congestive heart failure, and arrhythmias. A combination of metabolic dysfunction and increased cardiac workload from weight gain may lead to serious cardiovascular damage. If obesity is caused by a service-connected condition, such as PTSD or back injuries, then heart disease may be compensable as a secondary service-connected disability.
Heart disease may be eligible for ratings between 10%, 30%, 60%, and 100%, based on exercise tolerance, chest pain, and shortness of breath.
6. Respiratory Conditions
Obesity contributes to chronic respiratory issues like asthma, chronic obstructive pulmonary disease (COPD), and obesity hypoventilation syndrome (OHS). Excess weight compresses lung tissue and limits diaphragm movement, reducing airflow and oxygen exchange. Moreover, obese people may experience chronic cough, wheezing, or shortness of breath.
VA ratings for asthma range from 10%, 30%, 60%, to 100%, depending on pulmonary function tests, frequency of attacks, and treatment.
7. Depression, Anxiety, and Other Mental Health Disorders
Obesity and mental health issues are deeply interconnected, as restricted mobility, chronic pain, and social stigma can intensify depression, anxiety, or PTSD symptoms. Medications prescribed for mental health conditions can also trigger significant weight gain, creating a cycle that lowers overall functioning. Veterans should note that obesity and mental health share a two-way connection, where each can worsen the other, making this bidirectional relationship relevant in VA disability rating claims.
Mental health disorders are rated at 0%, 10%, 30%, 50%, 70%, and 100%, based on their level of occupational and social impairment.
Recognizing the Link Between PTSD and Obesity
This connection between obesity and PTSD is now recognized by the VA as a viable path for disability compensation through a secondary service connection. A survey of 3,157 U.S. veterans reported that 36% of veterans with probable PTSD were obese and 18% of veterans with obesity screened positive for probable PTSD, highlighting a bidirectional link between the two conditions (Sci Rep, 2020, Psychiatry Research).
For example, a veteran with service-connected PTSD may gain weight from medication or reduced activity tied to depression or anxiety. This intermediate obesity can cause sleep apnea, diabetes, or hypertension, allowing veterans to file for secondary VA disability claims under 38 CFR § 3.310.
How PTSD Contributes to Weight Gain
PTSD affects hormones such as cortisol, disrupting appetite, sleep, and motivation. Many cope through emotional eating, while reduced physical activity from fatigue or depression compounds weight gain. Additionally, psychotropic medications prescribed for PTSD, such as antidepressants or antipsychotics, are known to contribute to weight gain. Over time, this can result in obesity, which is clinically defined as a BMI of 30 or higher.
Veterans can establish a VA rating for obesity secondary to PTSD by showing:
- PTSD caused or aggravated their obesity,
- Obesity substantially contributed to a new condition (e.g., hypertension, joint pain, diabetes), and
- The secondary condition would not exist but for obesity.
Under 38 CFR § 3.310, a VA claim for obesity secondary to PTSD may support secondary ratings for:
- Sleep apnea
- Diabetes
- Hypertension
- Fatty liver disease
- Stroke or cardiovascular events
- Depression (or aggravated depression)
- Degenerative Joint Disease or Osteoarthritis
- Gastroesophageal Reflux Disease (GERD)
A well-supported nexus letter, clearly linking PTSD to obesity and showing how the extra weight caused or worsened secondary conditions, can bridge the gap. Veterans may even qualify for TDIU if these conditions limit employment.
TDIU and Obesity: When Weight Gain Impacts Employment
Total Disability based on Individual Unemployability (TDIU) allows veterans to receive compensation at the 100% disability rate when their service-connected conditions, directly or indirectly aggravated by obesity, prevent them from maintaining substantially gainful employment. This benefit recognizes that, while a veteran’s combined rating may not reach 100%, their actual ability to work may still be severely compromised.
To qualify, veterans must typically show either:
- One service-connected disability rated at least 60%, or
- Multiple disabilities, with one rated at least 40% and a combined rating of 70% or higher.
Obesity and related complications can create significant barriers to employment, for instance,
- Fatigue and daytime sleepiness from sleep apnea
- Severe joint pain limiting mobility
- Cardiovascular strain
- Depression that diminishes focus and motivation
If weight gain and related impairments substantially restrict job performance or attendance, veterans may qualify for TDIU, even without a schedular 100% rating.
Documentation That May Strengthen an Obesity-Related VA Claim
When you pursue VA disability for obesity, submitting comprehensive documentation can ensure a higher chance of claim approval.
1. Medical Records and BMI Evidence
- A confirmed medical diagnosis of obesity, having a body mass index (BMI) of 30 or higher
- Service treatment records showing a clear weight increase during active duty
- VA or private treatment records documenting ongoing weight gain, mobility limitations, and related conditions such as type 2 diabetes, arthritis, or sleep apnea.
- Evidence of prescribed medications or treatments to manage weight
2. Nexus Letters from Medical Experts
Perhaps the most critical piece of evidence in demonstrating obesity-related VA claims is a medical nexus letter. A sample nexus statement looks like,
“It is my professional medical opinion that it is at least as likely as not (50% probability or greater) that the veteran’s service-connected PTSD contributed substantially to the development of obesity.”
A well-written nexus letter will also cite scientific literature, explain medical reasoning, and connect the dots between obesity and secondary disabilities. You can strengthen your claim by obtaining an independent nexus letter from private medical specialists, offering unbiased and well-documented opinions.
3. Vocational and Functional Evidence
Since the VA evaluates how obesity impacts a veteran’s ability to earn a living, consider documenting functional limitations, such as:
- Difficulty walking, rising from a seated position, or maintaining balance.
- Records showing decreased endurance, chronic fatigue, or breathing problems.
- Employer statements or vocational assessments demonstrating lost earning capacity.
4. Lay and Buddy Statements
Finally, personal statements (VA Form 21-4138) and buddy letters from family, coworkers, or fellow service members add credibility. These accounts can describe how the veteran’s visible weight gain, lifestyle changes after injury, reduced activity, or emotional struggles tied to service contributed to obesity.
Together, this documentation establishes the essential link the VA looks for when deciding whether obesity and related disability are service-connected.
Case Study: Knee Injury Leading to Obesity and Diabetes
A veteran tore ligaments in his knee during service and was granted a 40% rating for chronic pain and instability. Over time, his limited mobility made it difficult to exercise. His weight rose to 245 lbs at 5’8” (BMI 37), eventually leading to Type 2 diabetes. The diabetes, consequently, brought nerve pain in his feet and vision problems that interfered with daily activities.
His doctor noted that the knee injury directly restricted activity, which caused obesity, which in turn led to diabetes and its complications. With a strong nexus letter, the VA recognized diabetes and neuropathy as secondary to the knee injury, with obesity as the crucial intermediate step, significantly increasing his overall rating and benefits.
What to Do If Your Obesity Claim Is Denied
VA generally denies obesity-related claims because veterans often lack a clear medical nexus showing that excessive weight is caused or aggravated by a service-connected condition.
If your VA claim for obesity as a secondary condition is denied, then choose an appeal option:
- Higher-Level Review
- Supplemental Claim or
- A direct appeal to the Board of Veterans’ Appeals
Submitting new and relevant evidence, like fresh medical nexus opinions, may bolster your case. Consider getting help from a Veterans Service Officer (VSO) or accredited representative to guide you through the appeal process.
Disclaimer: This article is meant for educational purposes only and does not constitute legal, medical, or professional advice. Veterans should consult qualified healthcare providers or accredited representatives before acting on VA disability claims related to obesity or associated conditions.
Navigating the Complex Terrain
Understanding the intricate connection between obesity and veterans’ disability requires careful consideration of medical history and the specific criteria outlined by the VA. Veterans seeking service connection for conditions associated with obesity should collaborate with accredited representatives to navigate this complex terrain. Each case is unique, and a comprehensive review of medical charts, supported by relevant evidence, is crucial in establishing the link between service-connected conditions, obesity, and subsequent disabilities. By fostering awareness and dialogue on this issue, veterans can better advocate for their rights and access the disability benefits they deserve.
FAQs
Is obesity eligible for a VA disability rating?
No, obesity is not a rateable VA disability on its own but can be used as an intermediate step to connect other service-related conditions.
Can obesity be secondary to PTSD?
Yes, obesity can be considered secondary to PTSD if the condition or its treatment causes significant weight gain leading to other disabilities.
Can I claim obesity as a VA disability?
You cannot claim obesity as a direct VA disability, but it may support secondary service connection or TDIU if it leads to functional impairments.
At what weight is obesity considered a disability?
Obesity is considered medically significant at a Body Mass Index (BMI) of 30 or higher, but VA does not rate it directly as a disability unless it causes functional impairment of earning capacity.
What are the secondary conditions related to obesity?
Common VA secondary conditions linked to obesity include sleep apnea, type 2 diabetes, hypertension, heart disease, orthopedic disorders, and mental health issues like depression or anxiety.
Can I get a VA disability rating for obesity secondary to PTSD?
While obesity itself is not rated, veterans may receive ratings for secondary conditions (e.g., sleep apnea, diabetes, hypertension) caused by obesity linked to PTSD, potentially qualifying for TDIU or increased compensation.
Also read: Nexus Letter for Secondary Condition: The Ultimate Guide (Sample Letter)
At Prestige Veteran Medical Consulting, a veteran-owned company, we specialize in Independent Medical Opinions (IMOs) known as Nexus letters.
Our purpose is to empower YOU, the veteran, to take charge of your medical evidence and provide you with valuable educational tools and research to guide you on your journey.
Understanding the unique challenges veterans face, our commitment lies in delivering exceptional service and support.
Leveraging an extensive network of licensed independent medical professionals, all well-versed in the medical professional aspects of the VA claims process, we review the necessary medical evidence to incorporate in our reports related to your VA Disability Claim.
Prestige Veteran Medical Consulting is not a law firm, accredited claims agent, or affiliated with the Veterans Administration or Veterans Services Organizations. However, we are happy to discuss your case with your accredited VA legal professional.