Last Updated on 1 September, 2025
Erectile dysfunction (ED) is a common yet often overlooked concern for veterans, particularly when it is linked to mental health conditions such as post-traumatic stress disorder (PTSD), depression, and anxiety. These connections not only affect a veteran’s quality of life but also play a critical role in determining eligibility for VA disability benefits.
In this article, Leah explores the relationship between ED and PTSD in the context of veterans’ disability claims, examining how service-connected conditions can contribute to erectile dysfunction and what veterans need to know when seeking compensation.

Table of Contents
PTSD and Erectile Dysfunction: What’s the Connection
Post-traumatic stress disorder (PTSD) is a chronic mental health condition that disrupts how the brain processes fear, stress, and emotions. Veterans living with PTSD often experience anxiety, depression, flashbacks, sleep disturbances, and emotional withdrawal. These psychological challenges, combined with the body’s heightened stress response, can significantly interfere with sexual health and contribute to erectile dysfunction (ED).
Research strongly supports this connection, and the correlation is widely recognized in the medical community and by the Department of Veterans Affairs (VA).
Why PTSD Leads to Erectile Dysfunction
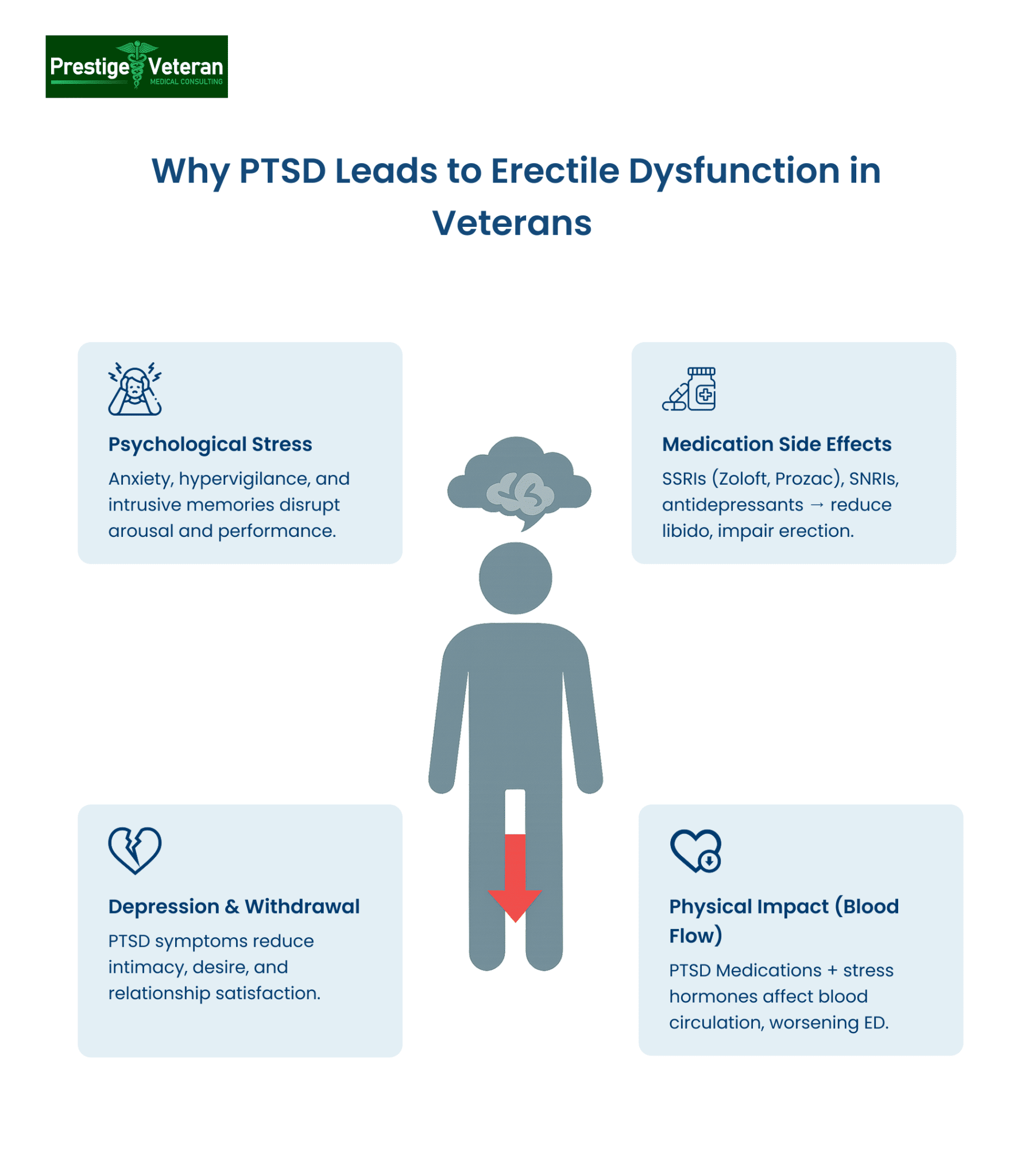
Several factors explain why veterans with PTSD are at a higher risk of ED:
- Psychological stress: Anxiety, hypervigilance, and intrusive memories disrupt arousal and sexual performance.
- Medication side effects: Antidepressants and anti-anxiety drugs, particularly SSRIs like Zoloft or Prozac, are known to lower libido and impair erectile function.
- Depression and emotional withdrawal: Core symptoms of PTSD may reduce intimacy, sexual desire, and relationship satisfaction.
This combination creates a “double burden,” where both PTSD itself and its treatment can trigger or worsen erectile dysfunction.
What Does “Erectile Dysfunction Secondary to PTSD” Mean?
When erectile dysfunction is claimed as secondary to PTSD, it means that the ED developed as a result of PTSD or was aggravated by it. This condition qualifies as a secondary service-connected disability under 38 CFR § 3.310, which states that any disability that is proximately due to or the result of a service-connected disease or injury is itself eligible for compensation.
This legal framework allows veterans to claim ED secondary to PTSD even if the sexual dysfunction wasn’t diagnosed during active duty. If the symptoms began or worsened after PTSD onset or treatment, veterans may still qualify for benefits.
For example, a veteran with a service-connected PTSD rating may later develop erectile dysfunction after years of chronic anxiety and prescribed antidepressant use. Since the sexual dysfunction arose as a direct result of the post-traumatic stress disorder and its treatment, it qualifies as secondary service-connected.
Service Connection for Erectile Dysfunction
Veterans can be service-connected for ED based on different circumstances.
Primary service connection occurs when the condition is directly related to service, meaning it was diagnosed and treated during active duty or otherwise developed during that time. This process is usually relatively straightforward if a valid diagnosis is established in service.
Secondary service connection, however, involves Erectile Dysfunction developing due to other service-connected disabilities. For instance, veterans with service-connected PTSD, diabetes, cardiovascular disease, prostate conditions, or spinal injuries may later experience Erectile Dysfunction. Certain medications prescribed for these conditions can also contribute to sexual dysfunction.
Whether Erectile Dysfunction is connected directly to service or arises secondarily, veterans are compensated for the unique impact the condition can have on quality of life, even if it does not produce a standard disability rating.
Research Evidence Linking PTSD and Sexual Dysfunction in Veterans
Secondary Service Connection and Mental Health Disorders
One common scenario leading to secondary service connection is Erectile Dysfunction related to mental health disorders. Numerous research articles support the link between PTSD, anxiety, and depression with sexual dysfunction in veterans. Notable studies include “Sexual Dysfunction: A Common Problem in Veterans with PTSD” and “PTSD and Sexual Dysfunction in Men and Women,” both published in the Journal of Sexual Medicine in 2015.
These studies highlight that male veterans with PTSD and anxiety are significantly more likely than civilian counterparts to experience ED and other sexual problems. In male combat veterans with PTSD, 85% reported erectile dysfunction, versus just 22% among those without mental health diagnoses. Female veterans also reported issues such as vaginal pain and disinterest in sex.
Utilizing such literature can strengthen a veteran’s case when applying for disability benefits related to secondary service connection.
Supporting Evidence: Peer-Reviewed Literature
Veterans can present peer-reviewed medical literature to their doctors or if they so choose, during Compensation and Pension (C&P) examinations. Articles like “Sexual Dysfunction and Selective Serotonin Reuptake Inhibitors and Potential Solutions: A Narrative Literature Review” highlight how SSRIs, commonly prescribed for PTSD, depression, and anxiety, are strongly associated with erectile dysfunction, decreased libido, and delayed orgasm.
By referencing credible clinical findings that demonstrate a well-established medical link between prescribed mental health treatments and sexual dysfunction, veterans can reinforce secondary service connection claims.
Medications and Erectile Dysfunction
It’s crucial to acknowledge that some medications prescribed for mental health disorders, such as selective serotonin reuptake inhibitors (SSRIs) and antipsychotics, may contribute to ED. The literature review mentioned earlier explores this connection, emphasizing the importance of considering the side effects of medications in disability claims.
In a population-based VA cohort of 405,275 OIF/OEF veterans, it was found that those with PTSD were more than three times as likely to experience sexual dysfunction, and the risk was even higher if they were prescribed psychiatric medications.
Common Medications for PTSD That Cause ED
Erectile dysfunction (ED) is a well-documented side effect of many medications prescribed to manage post-traumatic stress disorder (PTSD). Some popular PTSD medications that can contribute to ED include:
- Selective Serotonin Reuptake Inhibitors (SSRIs) like Sertraline and Fluoxetine are commonly used for PTSD and are frequently associated with sexual dysfunction, including ED.
- SNRIs like Venlafaxine (Effexor) may also impair sexual function by affecting neurotransmitters linked to arousal.
- Benzodiazepines (e.g., Ativan, Xanax), prescribed for anxiety or insomnia, can reduce libido and interfere with normal sexual response.
- Beta-blockers prescribed for anxiety or hyperarousal, are known to cause or worsen ED by affecting blood flow.
Veterans should ensure that prescription records are included in their medical evidence to support claims of ED secondary to PTSD medication.
Understanding VA Disability Ratings for PTSD
Post-Traumatic Stress Disorder (PTSD) is rated under 38 CFR § 4.130 (Schedule of Ratings, Mental Disorders), Diagnostic Code 9411. Ratings for this mental disorder depend on how severely symptoms affect work and daily life:
- 0% – Diagnosis, no functional impairment.
- 10% – Mild symptoms, usually controlled with medication.
- 30% – Occasional work/social impairment (depressed mood, anxiety, sleep issues).
- 50% – Reduced reliability and productivity (frequent panic attacks, memory/judgment issues).
- 70% – Deficiencies in most areas (suicidal thoughts, near-continuous depression, impaired impulse control).
- 100% – Total occupational and social impairment (hallucinations, danger to self/others, inability to function).
For veterans pursuing an Erectile Dysfunction claim, a granted PTSD rating of at least 10% provides the foundation for secondary service connection. Higher ratings (50%, 70% or 100%) indicate more severe impairment, which can strengthen the argument for TDIU benefits.
Proving Secondary Service Connection for Erectile Dysfunction Due to PTSD
To claim erectile dysfunction as secondary to PTSD, veterans must establish a secondary service connection under 38 CFR § 3.310, which grants benefits for a disability that is proximately due to or aggravated by an already service-connected condition.
To establish ED as a secondary condition to PTSD, veterans must provide three elements:
- A current medical diagnosis of ED – Documented by a licensed healthcare provider (urologist, VA doctor, or primary care physician) in medical records.
- Proof of Existing Service-Connected PTSD – An existing VA rating decision (typically 10% or higher) confirming PTSD is service-connected.
- Medical Nexus Linking ED to PTSD – A nexus letter from a qualified provider clearly explaining how ED is “at least as likely as not” (50% probability or greater) caused or aggravated by PTSD or its treatment.
In addition, veterans can strengthen their erectile dysfunction secondary claim with treatment records, prescription history, or statements from partners documenting changes in sexual function.
Special Monthly Compensation and VA Rating for Erectile Dysfunction Secondary to PTSD
Erectile dysfunction is typically rated at 0% under Diagnostic Code 7522 (38 CFR § 4.115b, Ratings of the genitourinary system) that now reads “Erectile dysfunction, with or without penile deformity — 0%”.
Note: VA finalized the genitourinary update in 2021 (see Federal Register summary)
What is Special Monthly Compensation (SMC-K) for Erectile Dysfunction?
Although ED is often granted a 0% non-compensable rating, that service connection opens the door for Special Monthly Compensation (SMC-K). This is a tax-free monthly benefit for veterans who have lost the use of a creative organ (including the penis or testicles).
- SMC-K Pay Rate (2025): $136.06/month
- Still Paid Even if Medications (like Viagra) are Effective
As of 2025, the SMC-K amount is $136.06 per month, and it is paid on top of your regular disability compensation, not instead of it.
See the official VA Special Monthly Compensation rates for the current amounts.
When Does ED Receive a Higher VA Rating?
While the standard VA rating for erectile dysfunction is 0%, higher ratings may apply if there are additional complications:
|
Diagnostic Code |
Condition |
VA Rating |
|
7522 |
Erectile dysfunction, with or without penile deformity |
20% |
|
7520 |
Removal of half or more of the penis |
30% |
|
7521 |
Removal of the glans |
20% |
|
7523 |
Atrophy of both testicles |
20% |
|
7524 |
Removal of both testicles |
30% |
For example, a veteran with service-connected PTSD develops erectile dysfunction and is granted a 0% rating. However, medical evaluations also show atrophy of both testicles, qualifying him for a 20% rating under Diagnostic Code 7523. In addition, he receives SMC-K at $136.06 monthly.
That means, the veteran’s total compensation would be:
- PTSD (50%) + Testicular Atrophy (20%) → 60% combined rating
- 60% rating = $1,395.93/month
- SMC-K = $136.06/month
- Total: $1,531.99/mo (rounds to $1,532)
All figures above come from 2025 VA disability compensation rates; SMC-K’s criteria and the genitourinary diagnostic codes are per the CFR. If the veteran has dependents, the base amount of the disability pay changes (SMC-K stays $136.06).
How to File a VA Claim for Erectile Dysfunction Secondary to PTSD
Veterans can file a claim for ED secondary to PTSD directly through the VA.gov website or by submitting VA Form 21-526EZ (Application for Disability Compensation). This claim should clearly state that erectile dysfunction is secondary to an already service-connected PTSD diagnosis.
Steps to File a Secondary Claim:
- Gather medical evidence:
- Current diagnosis of erectile dysfunction
- Proof of service-connected PTSD (rating letter from VA)
- Nexus letter linking primary PTSD or its treatment to secondary ED
- Log in to VA.gov and start a new disability compensation claim.
- List Erectile Dysfunction as a new condition, and specify it is secondary to PTSD in the description box.
- Upload supporting documents:
- Medical records
- Nexus letter from an independent medical provider
- VA and private treatment records
- Prescription history (especially if ED started after beginning PTSD medications)
- Lay statements or other evidence
- Submit the claim either through
- VA.gov online portal
- By mailing to your Regional Office, or
- In person at a local VA Regional Office (with or without the help of a Veterans Service Organization)
- Wait for a VA decision. Regularly check updates in your VA.gov account under the claims status section and respond quickly to any VA requests for information.
- Attend the Compensation & Pension (C&P) Exam scheduled by the Veteran Affairs to evaluate your ED symptoms and confirm secondary service connection.
Veterans can seek help from accredited VSOs (e.g., DAV, VFW, American Legion) or legal representatives experienced in VA disability claims to ensure all required documentation is complete and accurate.
How Does the VA Test for Erectile Dysfunction?
To evaluate erectile dysfunction for disability compensation, the VA will use a Compensation and Pension (C&P) exam, often using the Male Reproductive System Disability Benefits Questionnaire (DBQ).
During the evaluation, the VA examiner may:
- Review a veteran’s medical and mental health records
- Ask about your sexual history, frequency of symptoms, and functional impact
- Assess for sexual side effects related to PTSD or other prescribed medications
- Document any physical deformities, testicular atrophy, or other reproductive system problems
In many cases, an in-person exam for erectile dysfunction is not needed if the diagnosis and link to PTSD are clearly documented in your medical records and supported by a nexus letter.
Pro tip: Make sure your doctor notes any sexual side effects from PTSD or mental health medications, as this can help in proving that your ED is service-connected.
Total Disability Based on Individual Unemployability (TDIU) for Secondary Claim for ED
Veterans with PTSD and erectile dysfunction (ED) may qualify for Total Disability based on Individual Unemployability (TDIU) if their combined service-connected conditions significantly impact their ability to maintain substantially gainful employment. While ED is typically rated at 0%, it may still contribute to functional impairment when combined with severe PTSD symptoms such as anxiety, insomnia, flashbacks, or emotional numbness.
To qualify for schedular TDIU under 38 CFR § 4.16(a), a veteran must have:
- One service-connected disability rated at 60% or more, or
- Two or more disabilities with one rated at least 40%, and a combined rating of 70% or more.
For veterans who do not meet the schedular threshold, extraschedular TDIU under § 4.16(b) may still be pursued, especially if medical evidence shows that combined impairments, including ED secondary to PTSD, prevent gainful employment. Lay statements from spouses or former coworkers, or employees mentioning job difficulties, vocational assessments, and nexus letters can strengthen TDIU claims.
Example:
- PTSD rated at 70%
- Sleep apnea secondary to PTSD rated at 50%
- ED secondary to PTSD (SMC-K benefit)
With proper documentation and a strong medical nexus, a veteran may reach the threshold for schedular or extraschedular TDIU, qualifying for 100% VA compensation.
Case Study of a Marine Corps Veteran
Citation Nr: 20003191 – Decision Date: January 15, 2020
A Veteran served on active duty in the U.S. Marine Corps from January 1981 to March 1985. He testified before a Veterans Law Judge in January 2019, where his hearing transcript was added to the record. While the Veteran initially pursued an increased rating and an earlier effective date for his service-connected PTSD, those matters were resolved when a September 2019 decision granted him a 100 percent rating for PTSD for the full appeal period.
Issue: Entitlement to service connection for erectile dysfunction (ED) to include as secondary to service-connected PTSD.
What Supported the VA Claim for ED secondary to PTSD:
- Established PTSD Service Connection: The Veteran was already service-connected for PTSD, which included memory loss, alcohol abuse, and substance abuse in remission.
- Claim of Secondary ED: He consistently argued that his erectile dysfunction was secondary to PTSD, particularly as a side effect of prescribed PTSD medication.
- Medical Confirmation: A July 2015 VA male reproductive system examination confirmed the diagnosis of erectile dysfunction following review of medical history and a telephone interview.
- Contributing Risk Factors: The examiner noted the Veteran’s long-documented history of alcohol and cocaine misuse, both medically recognized as possible causes of erectile dysfunction.
While the examiner stated it would be speculative to determine the exact cause, the Board of Veterans’ Appeals emphasized that, for VA purposes, both the history of substance misuse and side effects of PTSD treatment were sufficient to establish a nexus.
Decision: Applying 38 C.F.R. § 3.310 (secondary service connection) and resolving doubt in the Veteran’s favor, the Board granted service connection for ED secondary to PTSD.
Source: Board of Veterans’ Appeals Decision, Citation Nr: 20003191 (Jan. 15, 2020)
Treatment Options for ED Secondary to PTSD
Veterans experiencing erectile dysfunction due to PTSD or related medication can access various treatment options through the VA or private providers. These include:
- Oral medications like Viagra (sildenafil) or Cialis (tadalafil)
- Vacuum erection devices (VEDs)
- Penile injections or implants (in advanced cases)
- Sex therapy or couples counseling
- Switching to PTSD medications with fewer sexual side effects
Veterans are encouraged to communicate openly with their mental health professional and a urologist to create a personalized treatment plan that considers both PTSD and erectile dysfunction.
Other Common Secondary Conditions to PTSD
Veterans with PTSD often suffer from multiple secondary conditions that are eligible for additional VA disability compensation under 38 CFR § 3.310. These include both physical and psychological impairments that are caused or worsened by the veteran’s primary service-connected PTSD.
Some of the most commonly accepted VA secondary conditions to PTSD include:
- Sleep Apnea Secondary to PTSD
- Chronic Fatigue Syndrome
- Depression or Anxiety
- Hypertension
- Substance Abuse
- Gastrointestinal issues (GERD, IBS)
- Female Sexual Arousal Disorder (FSAD)
All of these conditions may be claimed under secondary claims to PTSD by following the established VA framework:
Current medical diagnosis → Primary service-connected PTSD → Nexus letter linking the secondary condition to the primary disability
Tips to Increase Your VA Rating for Erectile Dysfunction Secondary to PTSD
There are important steps veterans can take to strengthen their claim and potentially qualify for a higher rating:
- Document All Symptoms and Complications – If ED is accompanied by testicular atrophy, penile deformity, or removal of testicles or glans, make sure these are documented in medical records. These conditions carry ratings from 20% to 30% under Diagnostic Codes 7520–7524.
- Get a Strong Nexus Letter – Ask a qualified physician (urologist, psychiatrist, or VA doctor) to clearly explain in a nexus letter that your ED is “at least as likely as not” caused or worsened by PTSD or its treatment.
- Include Prescription Side Effects – SSRIs, SNRIs, benzodiazepines, and beta-blockers are common PTSD medications that directly cause ED. Providing prescription history strengthens your claim.
- Submit Partner or Lay Statements – Statements from a spouse or partner describing the onset and impact of ED can provide valuable supporting evidence.
- Highlight Functional Impact – Explain how ED affects daily life, intimacy, and emotional health. Functional impairment evidence can tip the scales in your favor.
By gathering thorough medical documentation, nexus opinions, and lay evidence, veterans can move beyond a baseline 0% rating for erectile dysfunction and, where additional complications exist, qualify for higher compensation.
What if the VA Denies Your Claim?
If the VA denies a claim for erectile dysfunction secondary to PTSD, veterans have several options under the VA decision review and appeals process.
Veterans should consider filing a Supplemental Claim with new evidence or appealing to the Board of Veterans’ Appeals, where detailed, well-written nexus opinions frequently result in favorable outcomes.
Conclusion
In conclusion, veterans grappling with ED related to mental health disorders should be aware of the potential for secondary service connection and gather supporting evidence, including peer-reviewed literature and medical opinions. Understanding the VA rating system, the role of medications, and the possibility of SMC can empower veterans in their pursuit of disability benefits. It’s essential for veterans to consult with accredited agents, VSOs, or attorneys for guidance on the administrative process and ratings while utilizing available online resources like the 38 Code of Federal Regulations and VA.gov. By navigating these complexities, veterans can enhance their chances of securing the benefits they deserve.
FAQs
Is ED from PTSD a VA disability?
Yes, erectile dysfunction can qualify as a VA disability when it is proven as secondary to service-connected PTSD.
Can PTSD lead to erectile dysfunction?
Yes, PTSD can directly cause erectile dysfunction through psychological stress, depression, and side effects of medications.
Can you get VA disability for erectile dysfunction secondary to PTSD?
Yes, veterans can receive VA disability benefits for erectile dysfunction as a secondary condition to PTSD under 38 CFR § 3.310.
What is the average VA rating for erectile dysfunction?
Erectile dysfunction is usually rated at 0%, but veterans may receive Special Monthly Compensation (SMC-K) of $136.06/month in 2025.
Are PTSD and erectile dysfunction connected?
Yes, PTSD is closely connected to erectile dysfunction, with both the psychological effects of trauma and the side effects of common PTSD medications (like antidepressants) contributing to sexual difficulties.
What conditions can develop as secondary to PTSD for VA disability benefits?
Common secondary conditions to PTSD include sleep apnea, chronic fatigue, depression, anxiety, hypertension, substance abuse, gastrointestinal disorders, and sexual dysfunction.
Also read: How to Get VA Disability Benefits for Erectile Dysfunction
At Prestige Veteran Medical Consulting, a veteran-owned company, we specialize in Independent Medical Opinions (IMOs) known as Nexus letters.
Our purpose is to empower YOU, the veteran, to take charge of your medical evidence and provide you with valuable educational tools and research to guide you on your journey.
Understanding the unique challenges veterans face, our commitment lies in delivering exceptional service and support.
Leveraging an extensive network of licensed independent medical professionals, all well-versed in the medical professional aspects of the VA claims process, we review the necessary medical evidence to incorporate in our reports related to your VA Disability Claim.
Prestige Veteran Medical Consulting is not a law firm, accredited claims agent, or affiliated with the Veterans Administration or Veterans Services Organizations. However, we are happy to discuss your case with your accredited VA legal professional.














