Last Updated on 27 September, 2025
Veterans often find themselves facing Compensation and Pension (C&P) exams, a crucial step in the process of seeking benefits from the U.S. Department of Veterans Affairs (VA). Sleep apnea is the most commonly diagnosed sleep disorder among veterans, and navigating a C&P exam for this specific ailment can be a source of concern and confusion. So let’s find out the details of what to expect in a sleep apnea C&P exam, and provide insights into the process and the key aspects to ease veterans’ apprehensions.

Table of Contents
What Is Sleep Apnea and Why Is It Important to the VA?
Sleep apnea is a chronic sleep disorder where breathing repeatedly stops and starts during the night. There are three medically recognized types of sleep apnea, all of which the VA acknowledges for disability benefits:
- Obstructive Sleep Apnea (OSA): Caused by blocked or narrowed airways during sleep, leading to repeated pauses in breathing.
- Central Sleep Apnea: Occurs when the brain fails to send proper signals to the muscles controlling breathing.
- Mixed/Complex Sleep Apnea: A combination of both obstructive and central sleep apnea patterns in the same person.
Symptoms and Potential Risks in Veterans
Veterans might experience sleep apnea symptoms like loud snoring, waking up gasping for air, excessive daytime sleepiness, morning headaches, or difficulty concentrating. Many veterans develop or see their sleep apnea worsen because of service-related factors such as exposure to dust, burn pits, chemicals, high stress, or major weight changes after active duty.
If left untreated, sleep apnea can lead to serious health complications like high blood pressure, heart disease, or even stroke, so diagnosing it early matters.
To qualify for VA disability compensation, the VA requires a confirmed diagnosis through a sleep study (polysomnography). A diagnosis without a sleep study is usually not considered sufficient evidence for filing a VA claim.
The Purpose of the C&P Exam for Sleep Apnea
A Compensation and Pension (C&P) exam for sleep apnea is the VA’s formal evaluation of your condition. It helps determine three things:
- Confirm Diagnosis – Whether you have a documented sleep apnea diagnosis from a valid sleep study or private provider.
- Establish Service Connection – Determine if there is a direct, secondary, or presumptive service connection between your sleep apnea and military service.
- Assess Severity and Functional Impact – Evaluate the severity of your symptoms, including the need for a CPAP (Continuous Positive Airway Pressure) machine and how they affect your work, life, and social functioning.
In many cases, the VA may use the ACE (Acceptable Clinical Evidence) process for sleep apnea, letting examiners review existing medical records and complete the Disability Benefits Questionnaire without an in-person visit. If your evidence is insufficient, however, the VA will schedule you for an in-person evaluation instead.
Role in Veterans’ Disability Claims
The results of your C&P exam are crucial in determining your disability rating, as the examiner submits their findings to the VA rater rather than assigning a percentage directly. The VA rater then applies the 38 C.F.R. Part 4—Schedule for Rating Disabilities to decide your final rating, anywhere from 0% to 100%. Because of this, preparing carefully for the C&P exam is essential. Failure to attend or reschedule the exam promptly may impact your claim or even lead to denial.
Reporting to the Exam
When you receive notice for your C&P exam, it is likely that one of the three main contractors for C&P exams will conduct it. Although some exams may still be performed at VA facilities, outsourcing to contractors is becoming more prevalent. Veterans often receive information about their examiner beforehand, allowing them to research the examiner’s background and reviews if they wish. Examiners can be physicians, physician assistants, or nurse practitioners, depending on availability in your area.
Preparation and Paperwork
Before reporting to the exam, you may receive paperwork to fill out in advance. This documentation could include information about your symptoms, the history of your condition, and any relevant evidence. The examiner will likely have access to your claims file and other related documents to evaluate your history of the issue.
What Happens at a C&P Exam for Sleep Apnea
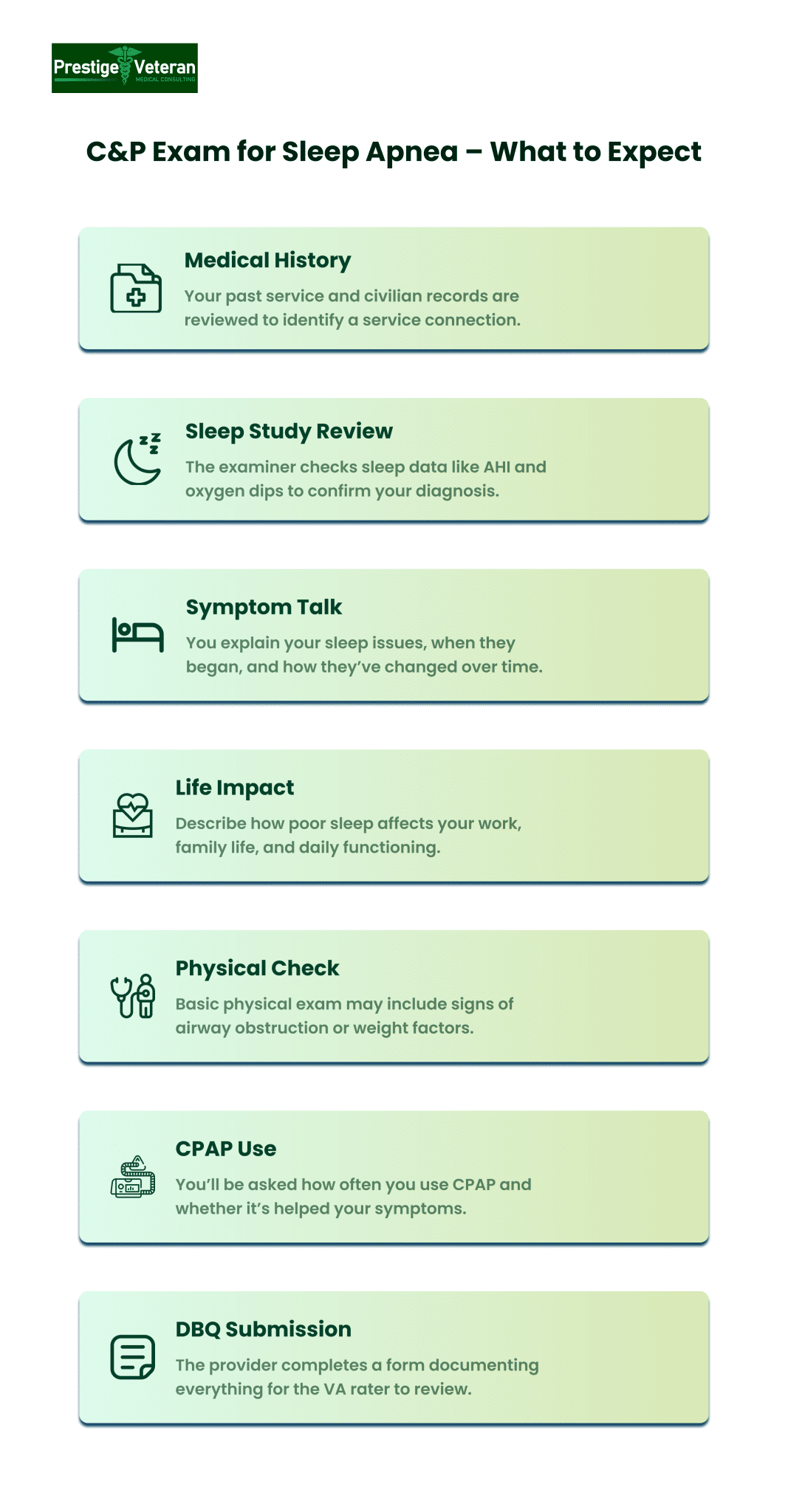
Whether conducted in person or as an ACE review, a sleep apnea C&P exam follows a structured approach. This VA examination can take 15–45 minutes, depending on the complexity of your case.
Review of Medical History
The examiner will begin by reviewing your medical history, focusing on service treatment records, post-service medical records, and any prior diagnoses. Bring key documents:
- VA or private sleep study reports
- BiPAP or CPAP prescriptions
- Physician treatment notes
- CPAP compliance logs
- Related conditions such as PTSD, obesity, GERD, or respiratory disorders
Sleep Study Review
If you have had a polysomnography (sleep study), the examiner will review data such as the apnea-hypopnea index (AHI) and oxygen saturation drops. This confirms the diagnosis and severity. Without a valid sleep study, the VA generally won’t grant service connection.
Discussion of Symptoms and Onset
Veterans will be asked to describe their apneic symptoms, such as:
- When symptoms began (snoring, gasping or dry mouth upon waking, headaches, fatigue).
- Whether symptoms started during or after military service.
- Use of CPAP or other breathing assistance devices.
- Daytime impairment, such as hypersomnolence or concentration problems.
You will be asked to describe how your military service may have contributed to the onset of your symptoms. Explain like, “I first noticed loud snoring and breathing interruptions during my 2010 deployment to dusty, high-stress conditions in Iraq. Since leaving the service, the symptoms have continued and now leave me exhausted during the day, requiring CPAP therapy.”
Impact on Daily Life and Work
The examiner must document how sleep apnea affects your daily functioning. Examples of functional impact may include falling asleep at work, difficulty operating machinery, irritability, and strained relationships due to loud snoring or mood changes. Be ready to explain how persistent fatigue interferes with your job performance, family life, and social interactions.
Physical Examination
During a sleep apnea C&P exam, the VA provider may evaluate the following aspects when conducting your physical examination:
- Signs of airway obstruction.
- Neck size, body weight, and other physical factors contributing to OSA.
- Adaptation to and compliance with a CPAP machine treatment.
Use of a CPAP device typically influences the disability rating for sleep apnea claims. Hence, you must explain the frequency, side effects, and whether your symptoms have improved with CPAP treatment.
Completion of the Disability Benefits Questionnaire (DBQ)
After the interview and exam, the provider completes the VA sleep apnea DBQ to document diagnosis, symptoms, treatment, and functional impacts. This DBQ form goes to the VA rater, who will evaluate your claim and decide your final disability rating.
Understanding the DBQ for Sleep Apnea
The heart of the C&P exam is often the Sleep Apnea Disability Benefits Questionnaire (DBQ), an official document examiners use to record various aspects of your condition. Knowing its structure helps you prepare your answers with relevant information.
Section I – Diagnosis
The first section of the DBQ requires specifying the type of sleep apnea (obstructive, central, mixed, or other) with diagnosis dates and ICD codes. It also confirms whether a sleep study was performed.
Section II – Medical History and Treatment
The examiner will inquire about the history of your sleep apnea, including when you first noticed symptoms, their progression, and course. The examiner notes whether continuous medication is needed, and whether a breathing assistance device (e.g. CPAP, mandibular device) is required for ongoing management.
You may discuss your experiences during service or any notable events reported by others, such as a spouse noticing breathing irregularities during sleep.
Section III – Findings, Signs & Symptoms
This DBQ section includes questions about specific signs and symptoms associated with sleep apnea, involving:
- Persistent daytime hypersomnolence,
- Carbon dioxide retention
- Chronic respiratory failure
- Cor pulmonale
- Tracheostomy
- Other relevant indicators
These signs capture how sleep apnea manifests physically, demonstrating its severity and relationship to VA rating criteria.
Section IV – Other Physical Findings & Complications
In this section, the C&P examiner will ask about additional related complications or signs tied to your sleep apnea diagnosis. They will also question whether any surgical or other treatment-related scars are present, noting their size, location, pain, or instability to give the VA a comprehensive picture of your disability.
Section V – Diagnostic Testing
The examiner reviews whether a formal sleep study was performed, and if so, whether that study shows documented sleep-disordered breathing. This section also lists any other relevant diagnostic tests you have undergone and their findings.
Section VI – Functional Impact
This section of the DBQ questions whether the sleep apnea impacts the veteran’s ability to work. If yes, the examiner should explain how by offering a few examples of reduced productivity, fatigue, lack of concentration, or safety risks provoked by the condition.
Section VII – Remarks
Finally, the examiner provides additional context or clarifications for the veteran’s case.
How the DBQ Affects Your VA Rating
The DBQ sleep apnea form directly influences your VA rating. For example, showing CPAP use in the form will typically meet the 50% rating threshold under current rules. Veterans who can demonstrate chronic respiratory failure or need for a tracheostomy may qualify for 100%.
You can download a VA sleep apnea DBQ PDF from the VA’s website or ask your own doctor to complete it before your C&P exam. In many cases, independent medical opinions or private DBQs can help counter an unfavorable VA exam.
Sleep Apnea C&P Exam Questions Veterans Should Know
When preparing for a VA Compensation & Pension (C&P) exam for sleep apnea, it helps to know the common questions examiners ask so you can clearly describe your symptoms, history, and daily limitations. Examiners frequently ask:
- When were you first diagnosed with sleep apnea via a private or VA sleep study?
- When did your symptoms begin, and how have they progressed?
- Do you use a CPAP or other breathing assistance device?
- How frequently and consistently do you use the device?
- How does sleep apnea affect your ability to work or perform daily tasks?
- Have you experienced severe complications such as daytime hypersomnolence or chronic respiratory failure?
- Did anyone in your unit, roommates, or family notice snoring or pauses in breathing during your service?
- Do you have other conditions (PTSD, weight gain, nasal issues) that might be related to or aggravate sleep apnea?
By reviewing these questions beforehand and bringing any supporting medical records or buddy statements, you can give more thorough, consistent answers that truly reflect how sleep apnea affects your life.
How to Prepare for Your Sleep Apnea C&P Exam
Thoroughly preparing for a sleep apnea C&P exam is important to ensure your condition is fully and accurately documented. Below are helpful tips to make the most of your appointment and support your VA claim effectively.
1. Gather and Organize Medical Evidence
In a C&P exam for sleep apnea, the examiner will verify your diagnosis and treatment history. Hence, gather and bring all relevant documentation to your appointment, including:
- Sleep study results
- CPAP prescription and compliance data
- List of current medications
- Any private sleep apnea DBQ forms completed by your doctor
- Physician notes
Submit these documents to the VA ahead of time and bring copies to your exam.
2. Keep a Symptom / Sleep Diary
Maintain a written log of your sleep patterns, CPAP usage, and any disruptions noted by a spouse or roommate for at least two weeks prior to your exam. Note symptoms like snoring, choking, waking up gasping or with a dry mouth, or excessive daytime fatigue.
This first-hand record illustrates the functional impact of your condition and strengthens the credibility of your VA sleep apnea claim.
3. Document Functional Impairments
List specific examples of how sleep apnea affects your daily activities, including missing work, falling asleep while driving, or mood changes that strain relationships. This aligns with the “Functional Impact” section of the DBQ.
4. Be Ready to Discuss CPAP or Other Devices
Clearly explain how often you use your BiPAP, CPAP (Continuous Positive Airway Pressure) machine, or other prescribed breathing device, including average nightly hours. Bring compliance reports to the examination. If you’re struggling, note any mask discomfort or side effects and describe how equipment use impacts your daily functioning.
5. Prepare Lay Statements (Buddy Letters)
If your spouse or roommate has observed your breathing interruptions, ask them to write a lay statement detailing what they have witnessed.
For example, your spouse may describe how you stop breathing in your sleep or how loud snoring wakes the household. A fellow service member might recall your excessive fatigue or napping during duty. These firsthand accounts provide valuable insights into the severity of your apneic episodes.
6. Review the DBQ Sleep Apnea Form
Familiarize yourself with each section of the Sleep Apnea DBQ in advance, focusing on questions about diagnosis, treatment history, and functional limitations. This preparation helps you give accurate, thorough answers that reflect the true impact of your condition on work, relationships, and daily life.
7. Be Honest and Consistent
Don’t minimize your symptoms. Provide statements like, “I’m exhausted all day from sleep apnea, and it cuts my work productivity in half.” Or else, “While driving my car, I’m genuinely scared of getting hurt or hurting someone else.”
Since the VA bases its decision on evidence and your statements, maintaining consistency between both may increase the chances of approval.
Conclusion and Medical Opinion
Following the detailed examination, the examiner will often offer a medical opinion. This opinion, however, may not be provided immediately during the exam. Instead, it is often submitted later, outlining whether the examiner believes your sleep apnea is related to your service. Importantly, the examiner’s opinion is just one piece of the puzzle, and the VA rater will consider the entirety of your case, including personal statements and any additional medical opinions.
VA Sleep Apnea Disability Ratings
Under 38 C.F.R. § 4.97, Diagnostic Code 6847, Sleep Apnea Syndromes (Obstructive, Central, Mixed), the VA currently assigns disability ratings for sleep apnea based on the severity and required treatment:
- 0% Rating: Diagnosis without symptoms.
- 30% Rating: Persistent daytime hypersomnolence (excessive sleepiness).
- 50% Rating: Requires use of a breathing assistance device such as a CPAP or BiPAP.
- 100% Rating: Chronic respiratory failure with carbon dioxide retention, cor pulmonale, or need for tracheostomy.
Because the use of a breathing assistance device (e.g., CPAP) is rated at 50% under the current DC 6847, maintaining compliance records is essential for claims and appeals.
Proposed changes (status): The VA has proposed significant changes to sleep apnea ratings under DC 6847 (87 FR 8474, Feb. 15, 2022). These include introducing a new 10% rating level, removing the current 30% level, and basing evaluations on veterans’ responsiveness to treatment rather than the treatment method itself. As of September 27, 2025, no final rule has been published in the Federal Register, so the existing criteria in 38 C.F.R. § 4.97 still apply.
VA Reexaminations for Sleep Apnea Claims
VA reexaminations for sleep apnea determine whether a veteran’s condition has improved, remained stable, or worsened since the initial rating decision. These follow-up Compensation & Pension (C&P) exams are often scheduled when the VA believes a disability may no longer meet the same criteria for benefits.
For example, a veteran initially rated at 50% for CPAP use may be reevaluated if compliance data suggests improvement. However, veterans over 55, those with stabilized ratings (five years or more), permanent disability status, or continuous ratings over 20 years are generally protected.
Explore how these rules apply in your case: VA 5, 10, and 20-Year Rules: Protect Your Disability Rating.
If scheduled, attend reexaminations and bring updated medical evidence to protect your VA claim from unfair rating reductions.
What to Do If Your VA Sleep Apnea Claim Is Denied
Understanding what to expect in a sleep apnea C&P exam is vital for veterans who may be seeking benefits. While the process may seem complex, veterans have options for appeal or review through the VA if the initial decision is not favorable. Veterans can:
- File a supplemental claim with new and relevant evidence (such as a private DBQ for sleep apnea or an updated nexus letter).
- Request a Higher-Level Review to challenge an unfavorable decision.
- Appeal directly to the Board of Veterans’ Appeals.
It is always best to discuss these matters with an accredited legal professional, like a veterans service officer or accredited attorney. By providing comprehensive information during the exam and supplementing it with supporting documents, veterans can enhance their chances of a fair assessment and a positive outcome in their pursuit of benefits.
FAQs
Do I need a C&P examination for sleep apnea?
Yes, if you file a VA disability claim for sleep apnea, the VA will generally require a Compensation & Pension (C&P) exam (or review via ACE) to properly evaluate your claim.
What are the new, proposed VA rules for sleep apnea?
Under the proposed 2025 changes, the VA will no longer automatically grant a 50% rating just for CPAP use, will introduce a 10% rating level (eliminating the 30% tier), and base ratings more on symptom severity, treatment effectiveness, and presence of comorbidities.
How does the VA test for sleep apnea?
The VA (or a qualified medical provider) requires an objective sleep study (polysomnography or comparable test) to confirm the diagnosis before granting disability benefits.
How to prove my sleep apnea VA disability?
You must submit a current diagnosis based on a sleep study, show continuity or service-connection (or secondary link), and provide a nexus opinion from a qualified medical professional.
What is included in the sleep apnea C&P exam?
During a sleep apnea C&P exam, the examiner will review your medical records and ask structured questions guided by the DBQ for sleep apnea.
What questions do they ask for a sleep apnea VA exam?
During a C&P exam for sleep apnea, expect questions about when your symptoms started, how they progressed, CPAP or other device use, daily limitations, and any related conditions or service exposures.
What is the DBQ form for sleep apnea?
The DBQ (Disability Benefits Questionnaire) for sleep apnea is a standardized VA form completed by the examiner that records symptoms, sleep study details, CPAP use, and functional limitations for rating purposes.
Also read: VA Sleep Apnea Ratings: 2025 Proposed Changes (and Current Rules)
At Prestige Veteran Medical Consulting, a veteran-owned company, we specialize in Independent Medical Opinions (IMOs) known as Nexus letters.
Our purpose is to empower YOU, the veteran, to take charge of your medical evidence and provide you with valuable educational tools and research to guide you on your journey.
Understanding the unique challenges veterans face, our commitment lies in delivering exceptional service and support.
Leveraging an extensive network of licensed independent medical professionals, all well-versed in the medical professional aspects of the VA claims process, we review the necessary medical evidence to incorporate in our reports related to your VA Disability Claim.
Prestige Veteran Medical Consulting is not a law firm, accredited claims agent, or affiliated with the Veterans Administration or Veterans Services Organizations. However, we are happy to discuss your case with your accredited VA legal professional.