Sleep apnea is one of the most frequently claimed disabilities among veterans, often linked to long deployments, weight changes, or respiratory exposures, and traumatic injuries. When filing for VA disability benefits, the rating you receive can feel confusing or even unfair. At the core of this process is Diagnostic Code (DC) 6847, the framework the VA uses to evaluate sleep apnea claims.
This blog walks you through the current DC 6847, explains how ratings are applied through real-world veteran examples, and why solid evidence can make all the difference in strengthening your claim.
Table of Contents
The VA’s Approach to Diagnostic Code 6847
Any sleep apnea rating analysis begins with 38 C.F.R. § 4.97, which outlines the VA’s rating schedule for the respiratory system. Under this regulation, Diagnostic Code 6847 governs the evaluation of sleep apnea claims and applies to obstructive, central, and mixed sleep apnea syndromes.
Currently, sleep apnea is not a presumptive condition under VA regulations. That means a veteran must show medical evidence of a current diagnosis, usually confirmed by a sleep study, and then link it to their military service or to another service-connected disability.
This service connection can be established in three paths:
- Direct service connection, where symptoms or diagnosis occurred during active duty.
- Secondary service connection, where sleep apnea develops as a result of another service-connected condition (for example, weight gain related to PTSD, chronic nasal obstruction from rhinitis, or a deviated septum).
- Aggravation, where a pre-existing condition was made worse by military service.
While evaluating sleep apnea claims, the VA is primarily concerned with both objective medical findings and the necessity of medical intervention. For example, a veteran prescribed a CPAP machine may typically receive a 50% rating, while documented daytime hypersomnolence may justify a 30% compensable rating.
The VA also considers the functional impact of sleep apnea, such as excessive daytime sleepiness, fatigue, or cognitive impairment, limiting job performance and overall quality of life.
By focusing on both medical documentation and real-world functional impact, veterans can better demonstrate the true severity of their condition under DC 6847.
VA Sleep Apnea Rating Criteria Explained
The Department of Veterans Affairs evaluates sleep apnea under the Schedule for Rating Disabilities in 38 C.F.R. § 4.97, Diagnostic Code 6847. VA assigns ratings of 0%, 30%, 50%, or 100%, based on symptom severity and the need for continuous positive airway pressure (CPAP) therapy or other assistive devices.
Under the current rating system, VA evaluates sleep apnea as follows:
- 0 percent — A sleep-disordered breathing diagnosis is documented but has no symptoms (i.e. asymptomatic) or is controlled without treatment. This establishes service connection but grants no monthly compensation.
- 30 percent — The veteran experiences persistent daytime hypersomnolence (excessive daytime sleepiness not relieved by rest). This rating level demonstrates ongoing but moderate impairment.
- 50 percent — Awarded when the veteran requires use (or prescription) of a breathing assistance device, such as a CPAP, BiPAP, or similar, demonstrating more serious functional limitations.
- 100 percent — The highest possible sleep apnea rating is reserved for the most severe cases involving chronic respiratory failure with carbon dioxide retention, cor pulmonale, or the need for a tracheostomy.
| VA Rating | Criteria (Under Current Rules) |
| 0% | Sleep study confirms apnea but asymptomatic |
| 30% | Ongoing excessive daytime sleepiness affecting work or daily function, but no CPAP prescribed |
| 50% | Medical prescription for CPAP, BiPAP, or similar breathing assistance device due to moderate or severe apnea |
| 100% | Chronic respiratory failure with CO₂ retention or cor pulmonale, or requires tracheostomy |
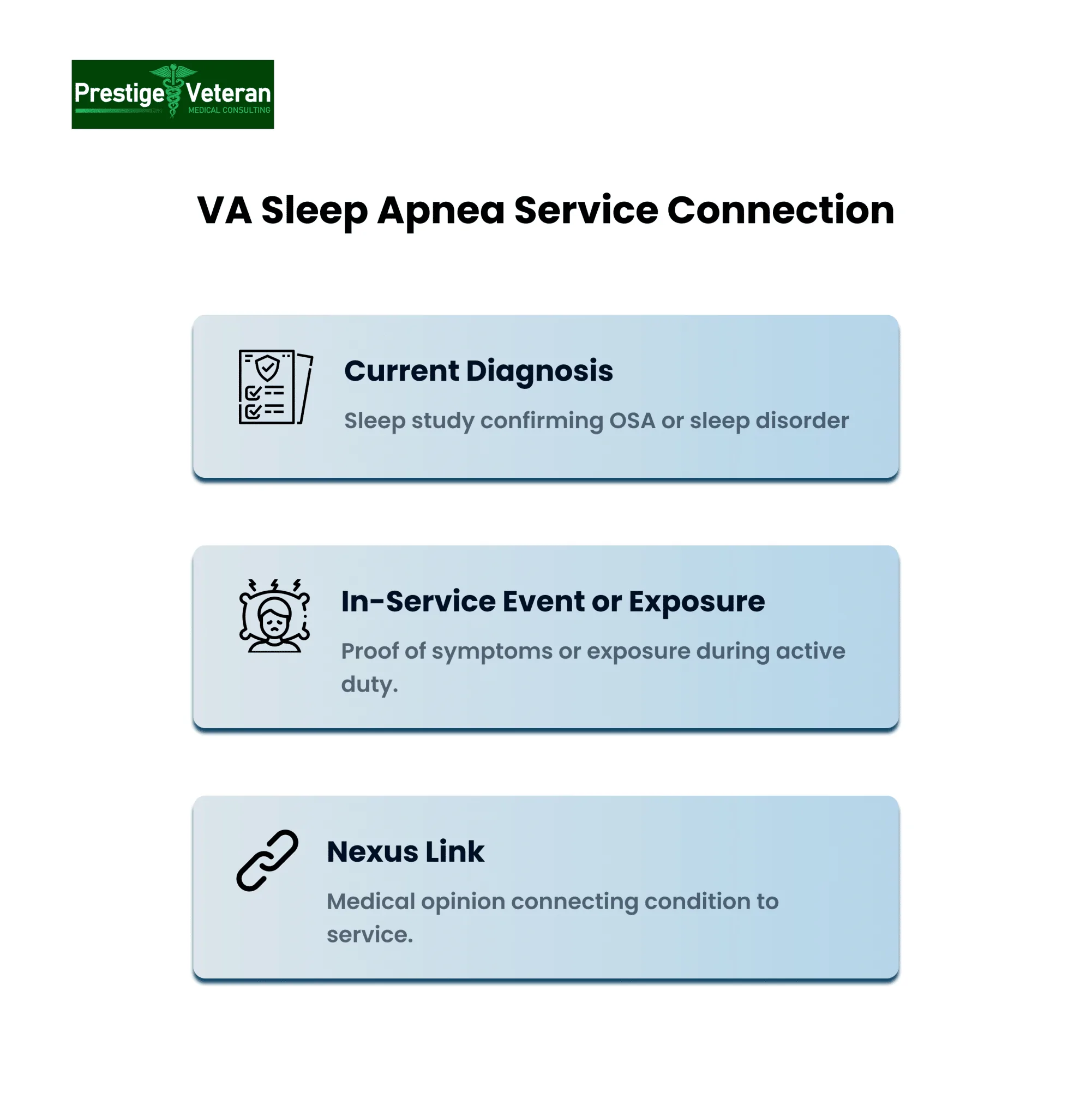
Three Requirements for Service Connection
To win a VA disability claim for sleep apnea, three core evidence elements must be present:
- Current Diagnosis: A valid sleep study showing obstructive sleep apnea (OSA) or another sleep-disordered breathing condition.
- In-Service Event or Exposure: Records or lay statements proving symptoms or conditions during active duty (snoring, daytime fatigue, respiratory hazards).
- Nexus Link: A medical opinion or expert statement clearly linking current diagnosis to military service or a secondary service-connected condition (like PTSD, obesity, or rhinitis).
How Sleep Apnea Ratings Under DC 6847 Affect Veterans
Understanding how VA applies Diagnostic Code (DC) 6847 is easier with real-world illustrations. These examples reflect how ratings progress from diagnosis to device use to complications, based on both objective testing and functional impairment.
0% Rating – Documented but No Symptoms
Derrick, a retired Marine mechanic, completes a VA sleep study showing mild obstructive sleep apnea (AHI = 8). He reports no daytime fatigue, drives commercially, and no device is prescribed. Because his apnea is documented but essentially asymptomatic, VA awards a 0 percent rating.
30% Rating – Persistent Daytime Fatigue Without CPAP
Maria, a former navy nurse, experiences ongoing daytime drowsiness and trouble staying awake at her desk. Her sleep study reveals moderate apnea (AHI = 20). Because her BMI and neck circumference suggested weight-related airway narrowing, her physician prescribed weight management instead of CPAP therapy. In this case, the VA grants 30 percent for persistent hypersomnolence.
50% Rating – CPAP Prescription Triggers Higher Rating
A Navy veteran’s sleep study confirms severe apnea (AHI = 35) showing symptoms like morning headaches, loud disruptive snoring, and frequent nighttime awakenings with gasping episodes. His partner noticed pauses in breathing during sleep.
As a result, his sleep specialist prescribes CPAP to prevent worsening symptoms. Even though the veteran occasionally removes the mask, the CPAP prescription alone qualifies him for 50 percent under VA criteria.
100% Rating – Serious Complications and Oxygen Therapy
Carlo, an Air Force retiree, develops chronic CO₂ retention and pulmonary hypertension from untreated severe apnea. He now needs continuous supplemental oxygen at night and during daytime naps. Because of these life-threatening complications requiring intensive intervention, the VA may boost his disability rating to 100 percent under DC 6847.
Understanding how VA raters apply DC 6847 helps veterans see where their condition fits on the rating scale and what evidence can prove their claim.
Evidence that May Support your VA Disability Rating Percentage
Once service connection is established, the VA assigns a disability rating based on the severity of sleep apnea. Below is a list of the evidence typically considered for each rating level.
0% Rating – Service-Connected but Noncompensable
A 0% rating means VA recognizes your sleep apnea is service-connected but considers it noncompensable at this time. This rating can still be valuable for access to VA health care and can be increased later if symptoms worsen.
- Sleep study confirming sleep-disordered breathing.
- Physician’s statement showing mild symptoms or effective treatment without daytime hypersomnolence
30% Rating – Persistent Daytime Sleepiness
- Sleep study showing mild or moderate OSA.
- Medical records and Epworth Sleepiness Scale scores showing daytime fatigue.
- Lay statements from spouse or coworkers describing naps, falling asleep at work, or concentration issues.
50% Rating – CPAP or BiPAP Prescription
- Durable medical equipment order or CPAP prescription.
- Original sleep study data supporting device use.
- Follow-up or usage notes (optional but persuasive).
100% Rating – Chronic Respiratory Failure
- Arterial blood gas test showing CO₂ retention.
- Echocardiogram or cardiologist note confirming cor pulmonale.
- Tracheostomy or continuous oxygen therapy records.
Tip: Strong lay statements from family members describing snoring, witnessed apneas, or daytime sleepiness can fill gaps in medical records and show the severity.
How VA Combined Ratings Affect Sleep Apnea Ratings
VA combined ratings directly influence the overall disability percentage awarded for veterans with sleep apnea. When a veteran has more than one service-connected condition, the VA Combined Ratings Table is applied rather than simply adding the percentages. This reflects how disabilities overlap in reducing a veteran’s overall health and functioning.
Service-Connected Conditions Secondary to Sleep Apnea
Many disabilities can be linked to or aggravated by sleep apnea, creating a pathway to secondary claims for veterans:
- Asthma
- Obesity
- Hypertension
- Sinusitis / Rhinitis
- GERD (Gastroesophageal Reflux Disease)
- Type 2 Diabetes Mellitus
- Mental Health Disorders (Depression, Anxiety, PTSD)
Example of How Combined Ratings are Calculated
A veteran rated 50% for sleep apnea, 20% for asthma, and 30% for chronic sinusitis/rhinitis:
- Start with the highest rating (50% for sleep apnea).
- 100% – 50% = 50% efficiency remaining.
- Apply the next rating (30% for sinusitis/rhinitis):
- 30% of the remaining 50% = 15%.
- 50% + 15% = 65% combined so far.
- Apply the third rating (20% for asthma):
- 100% – 65% = 35% efficiency remaining.
- 20% of 35% = 7%.
- 65% + 7% = 72% combined, rounded to 70%.
Final Combined Rating: 70%
Knowing this calculation helps veterans strategically plan secondary claims to potentially increase their overall VA rating and better anticipate their monthly compensation or eligibility for Total Disability Individual Unemployability (TDIU).
Automatic 50% Rating for CPAP and Its Impact
Under current VA rules, if a veteran is prescribed and required to use a CPAP machine, they automatically receive a 50% disability rating for sleep apnea if deemed service-connected on a causal basis. This rule is straightforward: the prescription itself triggers the rating, because VA sees CPAP dependence as proof of a chronic condition that cannot be managed without nightly medical assistance. Unlike the 30% rating, which only requires “persistent daytime hypersomnolence,” the 50% rating is objective, based on clear medical documentation rather than subjective symptoms.
Benefits of the 50% CPAP Rating
The implications are significant. A 50% rating can:
- Offers more than $1,000 a month for a veteran in 2025. This amount is higher when dependents are present. (View current VA disability compensation rates)
- Move veterans closer to TDIU or a combined 100% rating
- Guarantee ongoing coverage for equipment and supplies, reinforcing CPAP as a long-term, medically necessary treatment
The Debate and Proposed Changes
Still, this “automatic” rating has its critics. Some argue that veterans whose symptoms are fully controlled by CPAP may receive benefits that exceed their actual impairment. That concern is driving proposed regulatory changes that could shift focus from device use to functional limitations. Veterans who already hold the rating would likely keep it, but new claims after the changes may face tougher standards.
What Veterans Can Do to Qualify
For now, the rule is clear: a CPAP prescription equals 50% for required use. Veterans should keep thorough records, including:
- Medical device orders
- Invoices
- Follow-up notes to prove the ongoing prescription
Proposed VA Sleep Apnea Changes
As of September 30, 2025, the Department of Veterans Affairs (VA) has not finalized any new rules for rating sleep apnea. The VA first issued a Notice of Proposed Rulemaking on February 15, 2022 (87 FR 8474) and later released a Supplemental Notice on September 12, 2024 (89 FR 74162). According to the Federal Register, the proposed update shifts the focus from treatment devices like CPAPs to how sleep apnea functionally affects a veteran’s daily life.
Note that these are only proposals, not final regulations. Until the VA publishes a final rule and sets an effective date, the current criteria under Diagnostic Code (DC) 6847 still apply.
Proposed Rating Criteria:
| Proposed Rating | New Criteria |
| 0% | Asymptomatic, with or without treatment |
| 10% | Persistent symptoms despite effective treatment |
| 50% | Ineffective treatment or inability to use treatment due to comorbidities (no end-organ damage) |
| 100% | Ineffective or unusable treatment plus end-organ damage |
Key Changes
- Removes the automatic 30% rating currently tied to CPAP use.
- CPAP prescription alone will no longer equal a 50% rating.
- Adds 10% for partial relief, but ongoing symptoms.
- Retains 100% for severe cases, but only if both ineffective treatment and organ damage are documented.
Once finalized, the rule will outline effective dates and whether existing claims will be grandfathered. For now, treat any proposed rating tables as guidance only, not binding law. Veterans must consider submitting their claim before the proposed rules take effect to preserve access to the current, more generous criteria.
For a deeper breakdown of the proposed updates and what they could mean for your claim, see VA Sleep Apnea Rating Changes in 2025.
Practical Tips to Support Your VA Sleep Apnea Benefits
To support your case for VA disability benefits under Diagnostic Code 6847, veterans should take these proactive steps into consideration:
1. Consider filing claims early.
Submitting an Intent to File or a full VA sleep apnea claim now can secure the effective date and lock in the current, more favorable CPAP criteria before proposed rating changes take effect.
2. Get a current sleep study.
The VA often requires a sleep study to confirm your diagnosis and severity. Ask your provider for an overnight polysomnography if indicated.
3. Secure a CPAP prescription.
As documented, CPAP use is often the strongest path to a 50% VA rating for sleep apnea. Ask your VA or private doctor to prescribe CPAP if indicated. Pair objective records, such as sleep studies, CPAP prescriptions, or lab tests, with lay statements to build a persuasive VA claim.
4. Document symptoms continuously.
Keep daily logs of daytime fatigue, headaches, snoring episodes, mood changes, and naps. Ask spouses, fellow service members, or coworkers for written observations to support your VA claim with consistent, credible evidence.
Demonstrate how your sleep apnea began or worsened during service and continued afterward with consistent medical visits or treatment records.
5. Link the condition to service.
Obtain a medical nexus letter from a qualified provider connecting sleep apnea to documented in-service events such as exposure to burn pits or dust, PTSD, weight changes after deployment, nasal trauma, or snoring during active duty when applicable.
This independent medical opinion, written by a qualified physician, explains how your sleep apnea is “at least as likely as not” related to military service.
The nexus letter provider should use medical reasoning, cite evidence from your health history, and reference research linking these factors to sleep apnea development.
6. Be cautious about requesting increases.
Veterans with current VA sleep apnea ratings may be “grandfathered” under existing rules. Seeking a higher rating after the new criteria begin could unintentionally trigger a review, risking the reduction of already-protected benefits. It is always best to seek expert legal advice from an accredited legal professional when unsure of your options.
The stronger and more consistent your evidence, the higher your chance of receiving the VA sleep apnea rating you deserve.
If Denied, Don’t Get Discouraged
If the VA denies your sleep apnea claim, you can still build a stronger case. Many veterans succeed on appeal. First, carefully review the VA decision letter to see why the claim was denied. Missing nexus evidence, outdated sleep studies, or a lack of CPAP documentation are often common reasons for denial.
Veterans can respond by filing a Supplemental Claim with new evidence, requesting a Higher-Level Review, or appealing to the Board of Veterans’ Appeals with the assistance of an accredited legal professional. Veterans can also navigate this on their own, and there are helpful instructions regarding these options available at VA.gov.
Many successful veteran appeals depend on consistent documentation of symptoms and securing a clear nexus opinion from a qualified provider. Working with VA-accredited attorneys, Veterans Service Organization (VSO) or representatives who can handle complex legal and procedural requirements on your behalf, helps improve your claim outcomes significantly.
Conclusion
VA sleep apnea ratings can feel complicated, but with the right knowledge, you can approach the process with confidence. The key is knowing how Diagnostic Code 6847 applies, documenting your symptoms clearly, and staying on top of both current and proposed rules. Every rating percentage matters because it affects not only monthly compensation but also access to additional VA benefits and healthcare. If your initial claim or appeal feels discouraging, don’t hesitate to seek professional legal support. Remember, you have earned these benefits through service, so advocate for yourself.
FAQs
What is a 6847 VA rating?
A 6847 VA rating is the disability evaluation the VA assigns for sleep apnea under Diagnostic Code 6847, ranging from 0% to 100% depending on severity and treatment needs.
What is the new VA rating criteria for sleep apnea?
The proposed 2025 criteria would focus on functional impairment rather than CPAP use, adding a 10% tier and removing the automatic 50% rating for device prescriptions.
What is the DC code for sleep apnea?
The diagnostic code for sleep apnea is DC 6847, found in 38 C.F.R. § 4.97 under the respiratory system.
How to get a 50% rating for sleep apnea?
A 50% rating is usually awarded when a veteran is prescribed and required to use a CPAP, BiPAP, or similar breathing assistance device.
What are the VA criteria for sleep apnea?
The VA assigns 0% for asymptomatic sleep apnea, 30% for persistent daytime sleepiness, 50% for CPAP prescription, and 100% for chronic respiratory failure or tracheostomy.
Is it a mandatory 50% rating if issued a CPAP by the VA?
It is not strictly “mandatory” that issuance of a CPAP equals 50% in all cases, especially under the proposed changes, but under current rules, a CPAP prescription automatically qualifies a veteran for a 50% rating.
Why does the VA deny sleep apnea?
VA often denies claims due to a lack of a recent sleep study, missing nexus evidence, or insufficient proof linking the condition to military service.
What is the most common VA rating for sleep apnea?
The most common rating is 50%, since CPAP prescriptions are frequently granted for moderate to severe cases.
How to prove sleep apnea is service-connected?
To prove VA disability for sleep apnea, veterans must show a current diagnosis (sleep study), evidence of onset or worsening during or due to service or another service-connected condition, and a medical nexus opinion linking the two.
Also read: How to Win a Sleep Apnea VA Claim: 10 Effective Tips
At Prestige Veteran Medical Consulting, a veteran-owned company, we specialize in Independent Medical Opinions (IMOs) known as Nexus letters.
Our purpose is to empower YOU, the veteran, to take charge of your medical evidence and provide you with valuable educational tools and research to guide you on your journey.
Understanding the unique challenges veterans face, our commitment lies in delivering exceptional service and support.
Leveraging an extensive network of licensed independent medical professionals, all well-versed in the medical professional aspects of the VA claims process, we review the necessary medical evidence to incorporate in our reports related to your VA Disability Claim.
Prestige Veteran Medical Consulting is not a law firm, accredited claims agent, or affiliated with the Veterans Administration or Veterans Services Organizations. However, we are happy to discuss your case with your accredited VA legal professional.