Degenerative Disc Disease (DDD) is commonly diagnosed in veterans due to the physical strain endured during military service. It is an often painful spinal condition arising from the gradual wear and tear of spinal discs. Understanding how the VA rates DDD is crucial for veterans seeking disability benefits.
This guide explains VA rating criteria, service connection requirements, secondary conditions, and strategies to maximize your claim, assisting veterans in securing the compensation they rightfully deserve.
Table of Contents
What is Degenerative Disc Disease (DDD)?
Degenerative Disc Disease is not a disease, rather, it refers to the gradual breakdown of the intervertebral discs that cushion the bones of your spine. When these shock absorber discs wear down or dry out over time, they cause vertebrae to rub together and result in pain, limited mobility, and nerve compression.
Symptoms of degenerative disc disease include:
- Chronic lower back or neck pain
- Pain that worsens while sitting, bending, or twisting
- Radiating pain in the arms or legs
- Muscle spasms and stiffness
- Tingling, numbness, or weakness in the extremities
Although aging is a major contributor to DDD, it is important to recognize service-related spinal damage. Between 2001 and 2010, 131,986 active-duty U.S. service members were diagnosed with degenerative disc disease (DDD), meaning that for every 100,000 service members observed for a year, approximately 951 were newly diagnosed each year on average.
Why Veterans Are at Higher Risk for DDD
Military service often involves physical stressors like long-distance rucking, jumping from vehicles, and lifting heavy equipment over the years, which can accelerate spinal disc wear. This makes veterans especially vulnerable to developing DDD, even if symptoms don’t emerge until years later.
Consider a few common examples:
- Infantry soldiers often carry 60-100 lbs of gear daily, putting continuous strain on the lower spine.
- Paratroopers may experience hard landings that jar the spine and create long-term injuries.
- Mechanics and engineers often work in awkward positions, which can misalign spinal discs over time.
- Repeated physical training and conditioning cause repetitive stress that accelerates disc degeneration.
The VA disability for degenerative disc disease acknowledges that even if you weren’t diagnosed during active duty, the cumulative impact of military service can lead to long-term spinal conditions.
How the VA Rates Degenerative Disc Disease
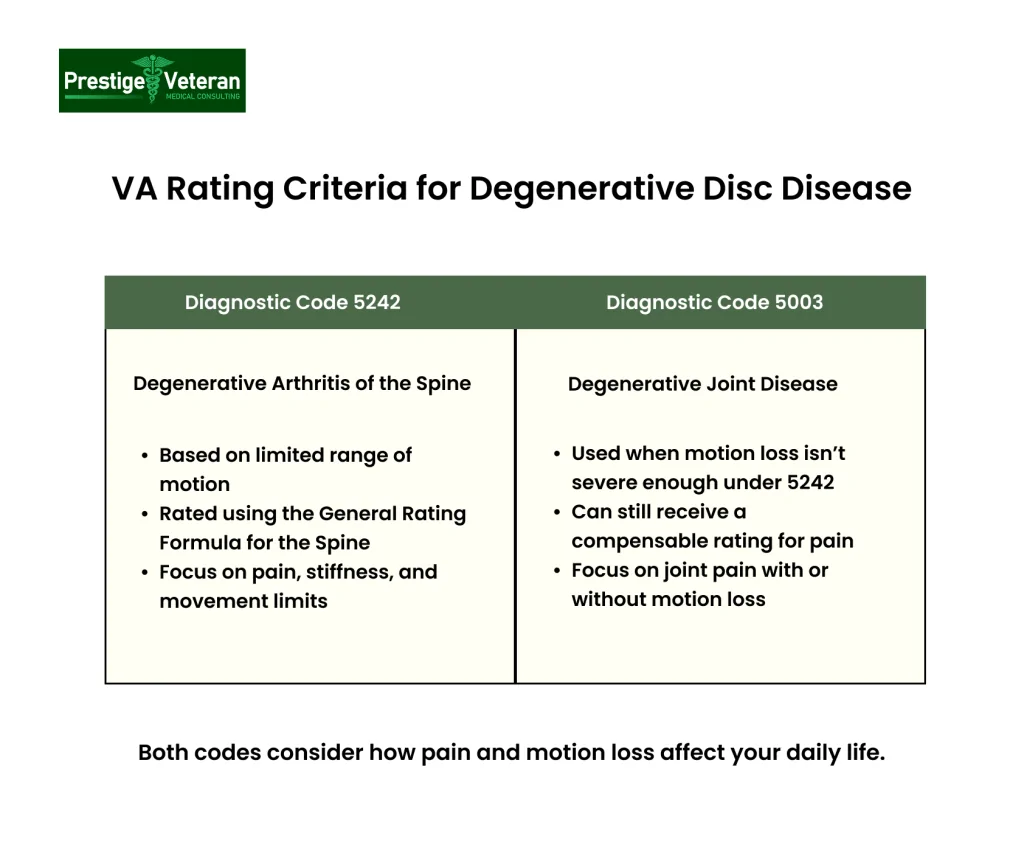
The VA usually assigns a disability rating for degenerative disc disease under one of two primary diagnostic codes.
- Diagnostic Code 5242: Degenerative arthritis affecting the spine
- Diagnostic Code 5003: Degenerative joint disease with limited range of motion
These codes focus primarily on range of motion (ROM) and how pain or stiffness impacts your daily functioning. If you have severe limitations in your ability to bend, twist, or extend your back or neck, your rating will likely be higher.
Pain alone can also result in a compensable rating under the VA’s “painful motion” rule, even if your range of motion appears normal during an exam.
Factors considered include:
- Degree of forward flexion
- Whether your spine is frozen (ankylosed)
- Evidence of muscle spasms or guarding
- How frequently you experience flare-ups or incapacitating episodes of pain
VA Rating Criteria for Degenerative Disc Disease Under DC 5003 (Degenerative Arthritis)
When DDD affects the spine, it is typically rated under Diagnostic Code (DC) 5242, which is used for degenerative arthritis of the spine. This code is part of the General Rating Formula for Diseases and Injuries of the Spine and evaluates the condition according to the extent of the veteran’s limitation of range of motion.
The VA ratings for degenerative disc disease vary from 10% to 100% depending on severity:
- 10% Rating: Limited spinal motion with minor flexion restrictions or localized tenderness/spasm without affecting gait or spinal alignment.
- 20% Rating: Moderate loss of spinal motion or muscle spasm/guarding causing abnormal gait or spinal curvature.
- 30% Rating: Severe cervical spine limitation with forward bending of 15 degrees or less, or unfavorable ankylosis of the entire thoracolumbar spine.
- 40% Rating: Forward flexion of the thoracolumbar spine limited to 30 degrees or less, or complete cervical spine ankylosis.
- 50% Rating: The entire thoracolumbar spine is fixed in an unfavorable (non-neutral) position.
- 100% Rating: Total spinal ankylosis involving both cervical and thoracolumbar regions.
Each percentage reflects how much your condition limits your ability to function and work. Understanding where your symptoms fall within these parameters is crucial to ensuring you receive the correct rating.
Degenerative Disc Disease Rating Under DC 5003 (Spine Conditions)
If your Degenerative Disc Disease (DDD) doesn’t meet the motion loss criteria under DC 5242, it may be rated under Diagnostic Code 5003 for degenerative arthritis based on X-ray evidence. This code falls under the Schedule of Ratings – Musculoskeletal System and is titled “Degenerative Arthritis, Other than Post-Traumatic.” It allows compensation for chronic symptoms such as pain or occasional flare-ups, even when joint motion is only mildly limited.
Breakdown of Rating Criteria:
- 10% Rating – Assigned for each major joint or group of minor joints showing limited motion, provided the limitation doesn’t qualify for a higher rating under another diagnostic code.
- 20% Rating – Granted when imaging test results confirm arthritis in two or more major joints or minor joint groups, with occasional flare-ups that impair function.
- 10% Rating – Also applicable when X-rays reveal arthritis in two or more major joints or minor joint groupings, but without evidence of incapacitating episodes.
Note that ratings under DC 5003 and DC 5242 cannot be combined for the same symptoms. When the spine is involved, DC 5242 typically takes precedence, meaning whichever rating is more appropriate or beneficial can be applied.
Proving Service Connection for Degenerative Disc Disease
To qualify for VA compensation, you must establish a service connection, the VA’s way of confirming your disability is tied to your military service. This involves three key elements:
- Current Diagnosis: You need a medical diagnosis of degenerative disc disease, confirmed by a qualified healthcare professional.
- In-Service Event: Evidence of an event, injury, or duty that could have caused or worsened your back condition (e.g., lifting heavy loads, a fall, or combat injury).
- Medical Nexus: A link between your current condition and the in-service event, typically written by a medical professional.
Buddy statements from fellow service members verifying the impact of your spinal pain during or after service can also be helpful. For veterans with existing VA disability, DDD can also be filed as a secondary service-connected condition, which we will discuss later.
Filing a VA Claim for Compensation
Many Veterans file VA disability claims for degenerative disc disease (DDD), by completing VA Form 21-526EZ, they often submit medical evidence of diagnosis and service connection, and file online through VA.gov, by mail, or at a VA regional office.
Conditions Secondary to Degenerative Disc Disease
Degenerative Disc Disease (DDD) often arises as a secondary condition to a primary service-connected disability, such as an injury to the knee, ankle, hip, or foot. These musculoskeletal impairments can alter your posture or gait, putting continuous stress on the spine. This ongoing strain often accelerates disc degeneration, particularly in the lumbar or cervical regions.
In addition to DDD itself, several conditions may develop as a result of spinal deterioration and can be claimed as secondary disabilities. When these are clearly documented and medically linked to your primary spinal condition, they can contribute to a higher combined VA disability rating and increase your total compensation.
Common secondary conditions of DDD include:
- Radiculopathy:
Radiculopathy occurs when degenerating discs compress spinal nerves, causing shooting pain, numbness, or weakness. Studies show disc herniation is a leading cause of lumbar and cervical nerve root impingement. - Spinal Stenosis:
Spinal stenosis occurs when the spinal canal narrows, often due to collapsed discs or excess bone growth, leading to compression of the spinal cord or nerve roots. - Spondylolisthesis:
Caused by weakened discs, this occurs when a vertebra slips forward over the one below, worsening pain and spinal instability. Degenerative spondylolisthesis is prevalent among older adults with disc degeneration. - Headaches:
Cervical disc degeneration can irritate upper spinal nerves, leading to cervicogenic or tension headaches that radiate from the neck to the head or shoulders. - Depression or Anxiety:
Chronic back pain and reduced physical function from DDD can lead to emotional distress, sleep issues, and mood disorders like depression or anxiety over time.
These conditions can be claimed separately or as secondary to your primary DDD rating. For instance, if you already have a 20% VA rating for disc disease and develop radiculopathy confirmed by a neurologist, you may receive an additional rating.
How Veterans often File a Secondary VA Claim for Degenerative Disc Disease
Veterans often file a VA secondary claim for DDD or any related conditions, and often provide strong supporting evidence, including:
- A current diagnosis of DDD and the secondary condition (supported by imaging test results like MRI or CT scans).
- Proof of a service-connected primary condition (e.g., ankle or knee injury).
- A nexus letter from a qualified medical provider clearly linking the primary condition to the development of DDD or associated complications. While this is never required, it can be helpful in some cases.
Thorough documentation can significantly improve your VA rating and ensure you receive the benefits you have earned.
Preparing for a C&P Exam for DDD
The Compensation & Pension (C&P) exam is a pivotal part of your VA disability claim for degenerative disc disease (DDD), as it directly influences your final VA rating. The sole purpose of this C&P examination is to verify the severity of your spinal pain symptoms and establish or deny a military service connection.
During the C&P exam, the VA-appointed examiner will assess more than your pain level. They will evaluate your spine’s range of motion using a goniometer to measure flexion, extension, etc., test for functional loss, and observe how symptoms such as muscle spasms, guarding, or abnormal posture affect your mobility.
To improve your chances of securing a favorable VA rating for disc disease, ensure you:
- Clearly describe flare-ups and how they affect daily living, e.g. difficulty standing, bending, or lifting and your ability to work.
- Bring a symptom journal or pain diary
- Stop movement as soon as pain begins during range-of-motion testing.
- Bring any relevant imaging (X-rays, MRIs) that show disc degeneration and treatments or therapies you are using.
- Mention secondary conditions (e.g., radiculopathy, anxiety, or related nerve issues).
Your exam results may contribute directly to your degenerative disc disease disability rating, with higher ratings possible in cases involving spinal stenosis, radiculopathy, or ankylosis. Whether your DDD affects your lumbar spine, cervical spine, or both, accurate documentation during the C&P exam ensures a fair evaluation.
Challenges to Getting the Right VA Rating for DDD
Receiving an accurate VA disability rating for degenerative disc disease can be frustrating. Many veterans face denials or low ratings due to gaps in documentation or misinterpretation of their symptoms.
Here are the main obstacles veterans face:
- Attribution to natural aging: The VA may claim your disc degeneration is age-related, not service-connected, even if your military duties clearly contributed.
- Lack of medical documentation: Without a diagnosis, medical nexus letter, or records from active duty, proving your condition is service-related becomes harder.
- Underrated symptoms: Veterans with pain, stiffness, or flare-ups may only secure a 10% or 20% rating, even if their condition is more severe.
- Dismissed flare-ups: If you don’t report episodic incapacitating pain or reduced functionality during flare-ups, they might not be factored into your rating.
What Veterans Can Do?
If your VA claim for degenerative disc disease is denied or underrated, you have the right to file a Higher-Level Review, a Supplemental Claim with new evidence, or appeal directly to the Board of Veterans’ Appeals. Consulting a VA-accredited representative can significantly improve your chances of receiving a fair disability rating.
TDIU Benefits for Degenerative Disc Disease
When your service-connected disc disease or related conditions make it difficult or impossible to hold a steady job, you may qualify for Total Disability based on Individual Unemployability (TDIU). TDIU allows disabled veterans to receive monthly payments at the 100% rate even if their combined rating falls below that threshold.
To qualify for full compensation through TDIU, you must meet one of the following:
- One service-connected condition rated at least 60% or higher, or
- Two or more service-connected conditions, with at least one rated at 40% and a combined rating of 70% or more.
You must also show that your service-connected DDD prevents you from maintaining substantially gainful employment. This applies to both physical and sedentary jobs; for example, pain from sitting, standing, or concentrating due to spinal issues can all qualify.
Supporting documentation to prove inability to work may include:
- Doctor’s opinion on inability to perform job duties
- Functional limitations described in C&P exams
- Employment history showing job loss or reduced hours
Example: A veteran with a 50% rating for cervical degenerative disc disease and a 30% rating for tension headaches struggles with constant neck pain and frequent migraines, making it hard to sit or focus at a desk job. With strong medical evidence and a history of job loss, they may qualify for TDIU at the 100% rate.
Securing a Favorable VA Rating for DDD
To maximize VA disability benefits for degenerative disc disease (DDD), veterans must present a thoroughly documented and compelling claim. Many veterans settle for a 10% or 20% rating when they may qualify for a significantly higher percentage, especially if the condition impairs mobility or employability.
Effective ways to support your VA benefits claim for DDD:
1. Obtain Detailed Medical Documentation
Diagnostic imaging, such as MRIs or CT scans, can confirm disc degeneration, bulging, or nerve compression, which are key factors in determining the severity of the condition.
2. Track Your Symptoms Consistently
Maintain a daily log of pain intensity, mobility limitations, flare-ups, and how these issues disrupt your work, sleep, and daily routine.
3. Request a Strong Nexus Letter
Ask your doctor to provide a detailed explanation linking your spinal condition to your military service, especially if your duties involved heavy lifting, impact trauma, or repetitive strain. For expert assistance in obtaining a compelling, medically sound nexus letter, consider consulting Prestige Veteran, a trusted resource for Independent Medical Opinions.
4. Include Lay Evidence
Statements from family, friends, or coworkers can illustrate how your DDD affects your everyday life and functionality.
5. Show Regular Treatment History
Ongoing physical therapy, chiropractic care, or pain management demonstrates the chronic nature of your condition and your commitment to managing it.
6. Claim All Possible Secondary Conditions
Degenerative disc disease (DDD) can lead to the development of various secondary conditions, such as radiculopathy, chronic pain–induced depression or anxiety, spinal stenosis, and scoliosis. These are eligible for separate ratings and can substantially increase your total disability compensation.
By thoroughly documenting every aspect of your condition and its effects, you improve your chances of elevating your VA rating from 10% to 20%, 40%, or more, reflecting the full scope of your disc disease.
Conclusion
Degenerative Disc Disease can significantly affect a veteran’s quality of life and ability to earn. Filing a strong, well-documented claim is key to receiving a fair VA disability rating. Use medical evidence, symptom tracking, and nexus letters to support your case. Seek professional guidance or legal help to appeal denied or underrated VA claims. Remember, even mild symptoms may warrant compensation if they affect your life. Be thorough, honest, and persistent in pursuing the VA benefits you have earned through military service.
FAQs
What is the highest possible VA rating for degenerative disc disease?
The maximum VA rating for Degenerative Disc Disease is 100% under Diagnostic Code 5242 when the entire spine is immobile due to unfavorable ankylosis. Whole ratings under Diagnostic Code 5003 are limited to a maximum of 20% when the condition doesn’t meet the criteria for limited motion.
How severe must degenerative disc disease be to qualify for VA disability?
You must have documented pain, limited range of motion, or functional impairment caused by DDD to receive a compensable VA disability rating.
Can you fully recover from degenerative disc disease?
No, degenerative disc disease is a chronic, progressive condition with no full cure, though symptoms can be managed.
Can I run with degenerative disc disease?
While possible in mild cases, running is sometimes discouraged for those with DDD due to its high spinal impact, which can worsen symptoms.
How difficult is it to obtain VA disability benefits for degenerative disc disease?
It can be challenging without proper documentation, but a strong medical nexus, symptom tracking, and secondary condition claims can greatly improve your chances.
What conditions are secondary to degenerative disc disease?
Radiculopathy, spinal stenosis, spondylolisthesis, headaches, depression, and anxiety are common conditions that often develop secondary to DDD.
What is the difference between intervertebral disc syndrome and degenerative disc disease?
Intervertebral disc syndrome (IVDS) refers to pain from a damaged disc, often due to herniation or irritation, while degenerative disc disease describes the gradual wear and tear of spinal discs over time.
Also read: Qualifying for a Lumbosacral Strain VA Disability Rating.
At Prestige Veteran Medical Consulting, a veteran-owned company, we specialize in Independent Medical Opinions (IMOs) known as Nexus letters.
Our purpose is to empower YOU, the veteran, to take charge of your medical evidence and provide you with valuable educational tools and research to guide you on your journey.
Understanding the unique challenges veterans face, our commitment lies in delivering exceptional service and support.
Leveraging an extensive network of licensed independent medical professionals, all well-versed in the medical professional aspects of the VA claims process, we review the necessary medical evidence to incorporate in our reports related to your VA Disability Claim.
Prestige Veteran Medical Consulting is not a law firm, accredited claims agent, or affiliated with the Veterans Administration or Veterans Services Organizations. However, we are happy to discuss your case with your accredited VA legal professional.