Sleep apnea is one of the most common disabilities affecting veterans, yet many are unsure how it fits into VA benefits or the PACT Act. With toxic exposures, combat stress, and service-related health issues, veterans face higher risks of developing this serious sleep disorder than civilians.
In this guide, we’ll discover whether sleep apnea falls under the PACT Act presumptive conditions list, how it relates to VA disability, burn pits, and what secondary conditions can help veterans build stronger disability claims. Whether you’re newly diagnosed or appealing a rating, the right knowledge empowers your next steps.
Table of Contents
Understanding Sleep Apnea and Its Impact on Veterans
Sleep apnea is a serious sleep disorder where breathing repeatedly stops and starts. Veterans may experience:
- Loud snoring
- Gasping for air during sleep
- Excessive daytime sleepiness (hypersomnolence)
- Irritability, headaches, or difficulty concentrating
There are three types of sleep apnea:
- Obstructive Sleep Apnea (OSA): Blockage of the airway
- Central Sleep Apnea (CSA): Brain fails to send proper signals
- Complex Sleep Apnea: Combination of OSA and CSA
Veterans are significantly more likely to develop sleep apnea than civilians. In a national study of 9.7 million U.S. veterans receiving care in the VA system from FY2000 to FY2010, sleep apnea was the most commonly diagnosed sleep disorder (47%), with its overall prevalence increasing six-fold during that period.
This may be due to a combination of military trauma, environmental exposure, and other service-connected conditions.
What Is the PACT Act?
The PACT Act, formally known as the Sergeant First Class Heath Robinson Honoring Our Promise to Address Comprehensive Toxics Act, is a groundbreaking law passed in 2022 to provide expanded benefits to veterans exposed to toxic substances, including burn pits, Agent Orange, and radiation.
Key benefits under the PACT Act:
- Expands VA healthcare eligibility for veterans exposed to toxins
- Adds over 20 new presumptive conditions related to burn pits, Agent Orange, and other hazardous exposures
- Recognizes more exposure locations, including Iraq, Afghanistan, and surrounding regions
- Requires the VA to conduct toxic exposure screenings for all enrolled veterans
The Act also enhances research and provider training around toxin-related illnesses, helping ensure veterans receive more timely, accurate diagnoses and care.
For veterans suffering from chronic respiratory or sleep-related symptoms, the PACT Act provides new grounds to explore potential service connections. This law represents a turning point in how toxic exposure claims, including those involving burn pits and respiratory health, are evaluated by the VA.
Is Sleep Apnea Presumptive Under the PACT Act?
No, sleep apnea is not a presumptive condition under the PACT Act as of 2025.
What Are Presumptive Conditions?
Presumptive conditions are medical issues that the VA automatically assumes are service-connected, meaning veterans don’t need to prove a direct link between their illness and military service. The PACT Act expanded this list to include over 20 conditions related to burn pit exposure in specified timeframes and locations, such as:
- Asthma diagnosed after service
- Chronic rhinitis or sinusitis
- Chronic obstructive pulmonary disease (COPD)
- Interstitial lung disease (ILD)
- Pulmonary fibrosis and other chronic lung conditions
However, sleep apnea is not included, despite its frequent co-occurrence with many of these respiratory issues.
What This Means for Veterans
If you’re suffering from sleep apnea and served in toxic exposure zones, you can still pursue VA disability, but you’ll need to establish a direct or secondary service connection.
How Burn Pit Exposure May Be Linked to Sleep Apnea
Understanding Burn Pits
Burn pits were widely used at U.S. military bases in Iraq, Afghanistan, and other locations to dispose of waste. They released a mix of harmful chemicals, including dioxins, particulate matter, and volatile organic compounds, which can irritate the respiratory system.
Are Burn Pit and Sleep Apnea Linked?
Research and veteran reports suggest a potential connection between burn pit exposure and obstructive sleep apnea (OSA). Toxins such as dioxins, benzene, and fine particulate matter inhaled by nearby troops over time may cause:
- Airway inflammation – leading to narrowed breathing passages during sleep
- Chronic sinus and lung issues – increasing the risk of disordered breathing
- Persistent respiratory symptoms such as coughing, wheezing, and shortness of breath
Recognizing Symptoms
Veterans exposed to burn pits should watch for symptoms of sleep apnea, such as loud snoring, daytime fatigue, morning headaches, and disrupted sleep.
Is Sleep Apnea a Presumptive Condition for Burn Pits?
Under the PACT Act, the VA automatically presumes that many post-9/11 veterans who served in Iraq, Afghanistan, and other listed areas were exposed to burn pit airborne hazards.
However, sleep apnea is not on the list of burn pit presumptive conditions. In other words, the VA does not automatically assume your sleep apnea was caused by burn pits. You still need a medical nexus opinion linking your diagnosis to service or toxic exposure.
See VA’s current presumptive lists for exposure to burn pits (eligible illnesses and duty locations).
Many service-connected respiratory illnesses already recognized as presumptive, such as chronic bronchitis, asthma, and COPD, can worsen or even trigger obstructive sleep apnea.
This means that while sleep apnea is not directly listed as a burn pit presumptive condition, medical evidence often shows a strong association.
VA Benefits and Testing
Veterans should work with healthcare providers and consider filing under the VA Airborne Hazards and Open Burn Pit Registry to document exposure and support their claims. Sleep studies and medical evaluations can also help confirm a diagnosis.
Understanding the medical link between burn pits and sleep apnea is vital for building a successful VA disability claim based on toxic exposure.
Sleep Apnea as a Gulf War Presumptive Illness
Technically, no. The VA does not currently recognize sleep apnea as a presumptive condition for Gulf War service under the PACT Act or other VA regulations.
However, there’s an important nuance.
Under 38 C.F.R. § 3.317, the VA does recognize “sleep disturbances” as a potential symptom of undiagnosed illnesses or medically unexplained chronic multisymptom illnesses (MUCMIs) eligible for presumptive service connection. While not a guaranteed path, this may allow some Gulf War veterans to argue their sleep apnea falls under that presumptive regulation, especially if no alternative cause is evident.
Despite not being automatically presumed service-connected for Gulf War Syndrome, veterans are statistically more likely to develop sleep apnea. A 2015 VA report found that sleep apnea was most prevalent among Gulf War-era veterans compared to other service groups.
Gulf War veterans can strengthen their sleep apnea VA claim with relevant evidence:
- Obtain a confirmed diagnosis through a sleep study
- Clearly document that symptoms began during or after service
- Provide a nexus letter linking sleep disturbances to Gulf War environmental exposures
Veterans may also establish a secondary service connection for sleep apnea, particularly if they already have a presumptive condition like asthma, chronic bronchitis, or sinusitis.
Then, How Can Veterans Service-Connect Sleep Apnea Through the VA?
To receive VA disability for sleep apnea, veterans must establish a service connection, which requires three elements:
- A current diagnosis confirmed by a sleep study (polysomnogram)
- Evidence of an in-service illness, event, or exposure (e.g., burn pits, trauma, airborne toxins, hazardous duty)
- Nexus letter—a medical opinion linking the condition to service
Sleep Apnea Can Be Service-Connected in Three Ways
Direct Service Connection
A direct service connection occurs when medical evidence shows a veteran’s sleep apnea began during active duty or was directly caused by a documented in-service event, illness, or exposure.
Example: A Gulf War veteran who was repeatedly treated for severe sinusitis and snoring while deployed develops obstructive sleep apnea soon after discharge. With a sleep study, supportive buddy statements, and an expert nexus opinion, this scenario can meet VA criteria for direct service connection.
Secondary Service Connection
Sleep apnea may develop as a result of another service-connected condition, including:
- PTSD
- Depression or anxiety
- Asthma
- Sinusitis or rhinitis
- GERD
- Obesity (linked to service-connected orthopedic or mental health conditions)
A secondary claim may be the strongest option for veterans pursuing compensation for sleep apnea as a service-connected condition. A nexus letter should clearly state that it is “at least as likely as not” that the primary condition contributed to or aggravated the veteran’s sleep apnea.
Aggravation of Pre-Existing Condition
If a veteran had undiagnosed sleep apnea prior to enlistment, but their condition worsened due to service-related factors, they may still be eligible for VA benefits based on aggravation.
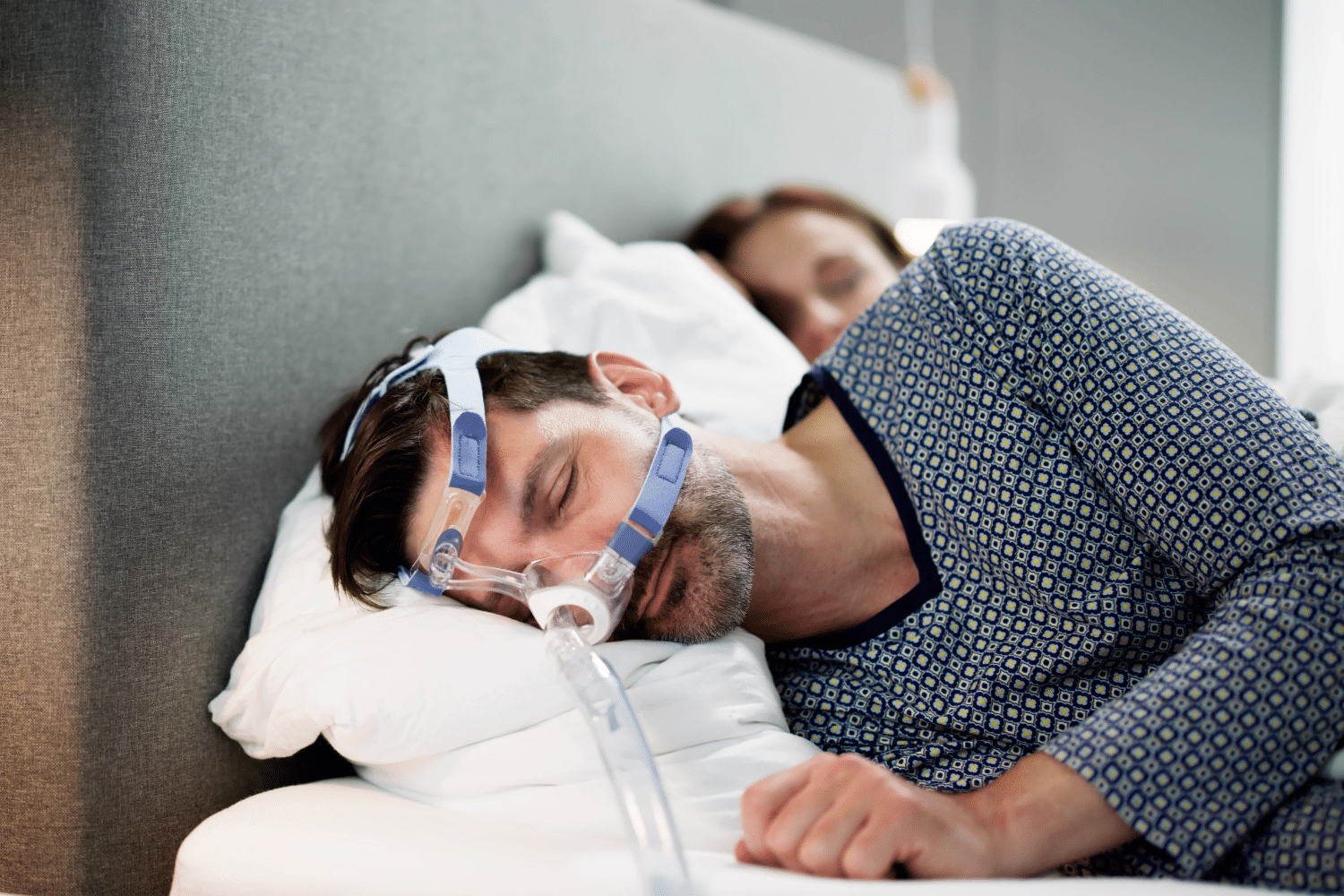
Example: Weight gain from a service-connected knee injury limiting physical activity could worsen pre-existing mild sleep apnea by increasing airway pressure, turning it into a severe obstructive sleep apnea case that needs CPAP therapy.
VA Disability Ratings for Sleep Apnea in 2025
The VA rates sleep apnea following 38 C.F.R. § 4.97 (Schedule of Ratings—Respiratory System), Diagnostic Code 6847. This code defines the specific criteria for 0%, 30%, 50%, and 100% disability ratings based on symptom severity and required treatment.
| Rating | Criteria | Monthly Compensation (2025) |
| 0% | Diagnosis confirmed, but no symptoms | $0 |
| 30% | Persistent daytime hypersomnolence | $537.42 |
| 50% | Requires a CPAP machine or another breathing assistance device | $1,102.04 |
| 100% | Chronic respiratory failure, CO₂ retention, or the need for a tracheostomy | $3,831.30 |
Most veterans receive a 50% rating when they require a CPAP machine.
If you have dependents, including a spouse, children, or parents, monthly compensation amounts may increase. See the VA’s official compensation tables for the updated payment rates.
Proposed Rating Changes in 2025
VA is considering rule changes that would make CPAP use no longer automatically qualify for 50%. Proposed criteria include evaluating the effectiveness of treatment (via sleep study), presence of end-organ damage, or inability to use the prescribed device due to comorbid conditions. The 30% rating might be removed, replaced with a 10% rating for incomplete symptom relief. Veterans currently rated will remain protected if these changes take effect.
Note: These changes are proposed, not in effect until a Final Rule appears in the Federal Register.
Want to know how these changes could impact your benefits? Read the full breakdown here.
Sleep Apnea as a Secondary Service-Connected Condition
Certain conditions often lead to or aggravate obstructive or central sleep apnea. When a veteran proves that their sleep apnea is secondary to one of these conditions, they may qualify for a VA disability rating, often at 50% if a CPAP is required or even higher if the condition is severe.
Here are some major service-connected conditions that can develop or aggravate sleep apnea:
- Post-Traumatic Stress Disorder (PTSD) – Chronic hyperarousal and stress from PTSD disrupts sleep patterns, which can increase airway muscle dysfunction.
- Asthma or Chronic Bronchitis – Airway inflammation from asthma or chronic bronchitis restricts breathing passages at night.
- Allergic Rhinitis or Chronic Sinusitis – Continuous swelling in the nasal passages reduces airflow, forcing irregular breathing patterns while sleeping, triggering sleep-disordered breathing
- Gastroesophageal Reflux Disease (GERD) – Acid reflux irritates throat tissue, which worsens airway inflammation and snoring.
- Obesity from Medications or Limited Mobility – Extra weight around the neck compresses airways during sleep and may exacerbate OSA or related issues.
- Traumatic Brain Injury (TBI) – Brain signal disruption from TBI can affect breathing reflexes, leading to central sleep apnea and poor sleep quality.
Example: A Gulf War veteran with presumptive asthma later develops obstructive sleep apnea requiring a CPAP machine. With a medical nexus letter clearly stating that it is “at least as likely as not” that the asthma-related inflammation caused or aggravated the OSA, the VA grants a 50% rating for sleep apnea on top of the veteran’s existing 30% rating.
This not only increases the veteran’s combined rating to 70% total monthly compensation but also qualifies them for Total Disability based on Individual Unemployability (TDIU) if their service-connected conditions prevent them from maintaining substantially gainful employment.
Hence, claiming an already service-connected condition remains one of the most effective paths to approval when sleep apnea itself isn’t presumptive.
Sleep Apnea and Vietnam Veterans: Exploring the Link
While the VA has granted presumptive status to many diseases linked to Agent Orange exposure, like Type 2 diabetes, ischemic heart disease, Parkinson’s disease, and various cancers, sleep apnea is not currently on this list. However, some emerging research suggests potential respiratory and neurological impacts from dioxin exposure.
In a study of 105 Vietnam‑era veterans with PTSD, about 69% had sleep-disordered breathing, which was highly associated with obesity.
That said, Vietnam veterans can still file for VA disability compensation for sleep apnea via direct or secondary service connection. For example, if a veteran has service-connected ischemic heart disease and a medical provider can show that it caused or worsened sleep apnea, the veteran may be eligible to file a secondary claim.
Additionally, veterans experience weight gain due to service-connected physical limitations or medications, which can also contribute to the development of obstructive sleep apnea.
Consulting an accredited Veterans Service Officer (VSO), attorney, or claims representative can help ensure your application includes the strongest possible medical and service evidence.
How to File a VA Claim for Sleep Apnea
Step 1 — Confirm the diagnosis. The VA will require a formal sleep study diagnosis confirming your obstructive, central, or complex sleep apnea.
Step 2 — Gather service evidence. Compile service records, deployment locations (especially burn pits), and buddy statements describing snoring, choking, or daytime fatigue in service.
Step 3 — Obtain a nexus opinion. Ask a licensed physician or specialist to explain how your service or a service-connected condition caused or aggravated your sleep apnea.
Step 4 — File the claim. Submit at VA.gov with VA Form 21-526EZ, by mail, or through assistance from a Veterans Service Organization (VSO). Upload the sleep study, nexus letter, CPAP compliance data, and lay statements.
Step 5 — Complete the C&P exam. Attend and fully participate in the Compensation and Pension (C&P) exam scheduled by the VA, as your disability rating depends on its results. Be consistent about describing your symptoms, CPAP use, and functional limits.
Step 6 — Track and respond. Track your status at VA Claim Status and answer any VA evidence requests promptly. If denied, consider a Supplemental Claim, Higher-Level Review, or Board Appeal with new evidence.
Why is a Nexus Letter Critical for Sleep Apnea Claims?
Because sleep apnea is not a presumptive condition under the PACT Act, veterans must provide robust medical evidence to bridge the gap between their diagnosis and service. This is where a medical nexus letter becomes powerful evidence. In the context of burn pit exposure, Gulf War environmental hazards, or linked secondary conditions, a nexus letter translates your exposure history and medical records into a clear, VA-friendly opinion.
Ideally, a well-written nexus letter may outline:
- Clear identification of your sleep apnea diagnosis (OSA, CSA, or complex) confirmed by a polysomnography
- Service locations and deployment records showing toxic exposure or high-risk environments
- Timeline of symptom onset during or after military service and relevant comorbidities
- Explanation of how service-connected conditions (if any) caused or aggravated your sleep apnea
- Citations to VA diagnostic codes and medical research linking your exposures to sleep-disordered breathing
- A nexus statement using VA’s “at least as likely as not” standard
By meeting VA’s evidentiary standards, a detailed nexus letter dramatically improves approval odds and can offset the lack of presumption, making it a cornerstone of your claim strategy.
Providers like Prestige Veteran Medical Consulting specialize in nexus letters or independent medical opinions tailored for veterans’ disability claims.
Winning Your Sleep Apnea VA Claim (Even Without Presumption)
Many veterans assume the PACT Act made sleep apnea automatically service-connected. It did not. While the Act expanded presumptions for burn pits and other toxic exposures, sleep apnea is still evaluated on a case-by-case basis. The key to winning VA disability for sleep apnea is evidence that directly links your condition to military service or to an already service-connected disability.
1. Understand Presumptive vs. Direct Service Connection
Although sleep apnea is not a presumptive VA disability, Gulf War regulations do allow certain “sleep disturbances” as undiagnosed illnesses. If you served in Southwest Asia or near burn pits, you may still argue for a sleep apnea Gulf War presumptive status or file as a direct or secondary condition.
2. Establish a Clear Symptom History
Gather in-service and post-service medical evidence, including:
- Lay statements from spouses, roommates, or fellow service members describing snoring, gasping, or daytime fatigue during active duty.
- Service treatment records, separation physicals, and early post-service medical notes.
- Weight changes or duty restrictions that could indicate the onset or aggravation.
3. Document Exposure Risks
Many studies show higher rates of obstructive sleep apnea among veterans exposed to toxins. Even though sleep apnea is not presumptive under the PACT Act, you can argue direct or secondary service connection by showing exposure to burn pits, airborne hazards, or Agent Orange.
To show increased exposure risk to hazardous toxins, you can submit:
- Deployment records
- Airborne Hazards and Open Burn Pit Registry entries
- Medical literature linking exposures to respiratory impairment
4. Request a High-Quality Medical Nexus Letter
A persuasive nexus letter from a qualified medical professional often bridges the gap between your service history and your diagnosis, especially in non-presumptive cases. More importantly, the nexus opinion should clearly state that your sleep apnea is “at least as likely as not” related to your military exposures or to other service-connected conditions.
5. Be Prepared for a C&P Exam
If the VA schedules a Compensation & Pension (C&P) exam, show up with your CPAP prescription and usage logs, medical evidence, and lay or buddy statements. Be ready to describe your symptoms, onset timeline, and how your condition affects daily life and employment. This exam is often the deciding factor in your claim.
6. Understand Proposed Rating Changes
The VA has proposed new rules that could affect the CPAP VA disability rating. Veterans already rated under current standards will be protected, but understanding future criteria can help when submitting new or supplemental claims. Acting before changes are finalized may preserve higher benefits.
7. Include All Secondary Conditions
When filing for VA disability for sleep apnea, consider any related conditions, GERD, PTSD, sinusitis, or asthma, that could demonstrate a secondary link. Veterans with a primary condition already recognized by the VA may qualify for an additional or higher combined rating for sleep apnea.
Ensure all documentation and evidence in your VA claim file is consistent and credible. Submitting a complete claim package reduces delays and greatly improves your chances of winning VA benefits, even if there’s a lack of presumption.
Appeal if Denied: What are the Options?
Most sleep apnea claims are first denied for a lack of formal diagnosis, in-service evidence, or nexus opinion. For securing a favorable outcome, you can:
- Submit a supplemental claim with new evidence, e.g. updated nexus letters, lay statement, or a completed DBQ (Disability Benefits Questionnaire).
- Request a Higher-Level Review.
- Appeal directly to the Board of Veterans’ Appeals.
Also, partnering with accredited representatives or attorneys familiar with VA regulations can help win appeals. They can gather well-documented evidence, present legal arguments, and ensure timely submission at each stage of the process.
Future of Sleep Apnea and the VA: Will It Become Presumptive?
As of 2025, sleep apnea is not considered a presumptive condition by the VA, even under the PACT Act. However, advocacy groups continue pushing for it to be added, especially for veterans exposed to burn pits or other toxic substances. Studies increasingly show links between sleep apnea and service-connected conditions like PTSD, TBI, and respiratory illnesses caused by environmental exposures. Moreover, entries in the Airborne Hazards Registry can help shape future VA policies by documenting exposures.
The VA is reviewing this growing body of evidence but has concerns about rising costs and overdiagnosis. At the same time, changes to the VA’s rating schedule are being proposed, which may reduce ratings for veterans whose symptoms are controlled with CPAP or similar devices. Because of this, veterans are encouraged to file claims now, before new rules take effect.
While sleep apnea isn’t presumptive yet, the VA may recognize it in the future as science and advocacy continue to evolve. For now, a clear medical nexus is still required when filing a claim.
Final Thoughts: Can Veterans Still Get Compensation for Sleep Apnea?
Although sleep apnea is not currently presumptive under the PACT Act, veterans still have options to establish service connection and secure the benefits they’ve earned. By documenting your diagnosis, linking symptoms to service or a secondary condition, and gathering strong medical evidence, you can improve your chances of approval. With preparation and expert guidance, veterans can build favorable claims and obtain higher compensation. Stay informed about evolving VA policies and advocacy efforts to act quickly if future presumptive changes occur.
Frrquently Asked Questions (FAQs)
Is sleep apnea a Gulf War presumptive?
No, sleep apnea is not officially a Gulf War presumptive condition, though “sleep disturbances” may qualify under undiagnosed illness rules.
Is sleep apnea presumptive for VA disability under the PACT Act?
No, as of 2025, sleep apnea is not listed as a presumptive condition under the PACT Act. Veterans must prove direct, secondary, or aggravated service connection for sleep apnea to receive VA disability benefits.
Will sleep apnea become presumptive?
Not yet, but advocacy and research may lead the VA to add it as a presumptive condition in the future.
Is sleep apnea a presumptive condition for burn pit exposure?
No, the VA does not automatically presume burn pit exposure causes sleep apnea, so a medical nexus is still needed.
When is the effective date of the VA sleep apnea changes?
The effective date of any VA sleep apnea rating changes has not been finalized and will be published in the Federal Register once officially approved.
How to win a sleep apnea VA claim?
Get a confirmed diagnosis, document in-service exposure or symptoms, and provide a strong nexus letter linking sleep apnea to service or a service-connected condition.
Is sleep apnea a permanent condition?
Sleep apnea is generally considered a chronic, ongoing disorder, but it can improve or worsen depending on treatment and health changes.
Also read: Nexus Letter for Sleep Apnea Secondary to PTSD (Example Included)
At Prestige Veteran Medical Consulting, a veteran-owned company, we specialize in Independent Medical Opinions (IMOs) known as Nexus letters.
Our purpose is to empower YOU, the veteran, to take charge of your medical evidence and provide you with valuable educational tools and research to guide you on your journey.
Understanding the unique challenges veterans face, our commitment lies in delivering exceptional service and support.
Leveraging an extensive network of licensed independent medical professionals, all well-versed in the medical professional aspects of the VA claims process, we review the necessary medical evidence to incorporate in our reports related to your VA Disability Claim.
Prestige Veteran Medical Consulting is not a law firm, accredited claims agent, or affiliated with the Veterans Administration or Veterans Services Organizations. However, we are happy to discuss your case with your accredited VA legal professional.