Last Updated on 24 September, 2025
Sleep apnea and Post-traumatic Stress Disorder (PTSD) often co-occur in veterans, creating a complex relationship that impacts veterans’ health and well-being. Characterized by breathing interruptions while sleeping, sleep apnea is common among veterans as a secondary condition to PTSD. A well-documented nexus letter can become essential in some cases for establishing this connection in VA disability claims.
According to the latest Fiscal Year Annual Benefits Report, more than 659,335 U.S. veterans have service-connected sleep apnea for which they receive disability compensation from the Department of Veterans Affairs.
In this insightful blog, we’ll explore the connection between PTSD and sleep apnea, understand the role of VA nexus letters (with a real-life example) in establishing the secondary service connection, and share what evidence veterans can provide to secure the benefits they deserve.
Table of Contents
Prevalence of Sleep Apnea and PTSD in Veterans
Sleep apnea is a condition where breathing repeatedly stops and starts, disrupting normal sleep patterns. It can lead to serious health problems, including cardiovascular disease, hypertension, and excessive daytime sleepiness. The American Lung Association estimates that over 30 million adults in the U.S. suffer from obstructive sleep apnea, making it a common disorder.
Veterans typically suffer from the following types:
- Obstructive Sleep Apnea (OSA): Blockage in the airway due to relaxed throat muscles.
- Central Sleep Apnea (CSA): The brain fails to signal the muscles responsible for controlled breathing.
- Complex Sleep Apnea: A combination of OSA and CSA, often emerging after treatment with a continuous positive airway pressure (CPAP) machine.
On the other hand, PTSD is a mental health condition resulting from traumatic experiences during military service. Veterans with post-traumatic stress disorder often deal with the following:
- Nightmares and flashbacks
- Hypervigilance and chronic stress
- Insomnia and poor-quality sleep
The connection between the two conditions lies in their overlapping symptoms. A study of 195 Iraq and Afghanistan veterans found that 69.2% were at high risk for sleep apnea, and the likelihood was greater for those with more severe PTSD symptoms.
How PTSD Contributes to Sleep Apnea
Veterans who claim sleep apnea secondary to PTSD often require well-documented medical research to substantiate their service connection. Several PTSD-related factors can directly or indirectly contribute to the condition:
Chronic Stress and Hyperarousal
Post-traumatic stress disorder keeps veterans in a constant state of “fight-or-flight,” which can disrupt normal breathing patterns during sleep. This heightened stress increases the likelihood of OSA.
Weight Gain from PTSD Medications
Many medications prescribed for PTSD management, including antidepressants and antipsychotic medications, can cause weight gain in veterans. Excess weight is a significant risk factor for obstructive sleep apnea because it increases pressure on the airway.
Sleep Fragmentation and Insomnia
Post-traumatic stress disorder (PTSD) disrupts REM sleep through frequent awakenings, nightmares, and insomnia. This disturbance impairs the brain’s ability to process and regulate traumatic memories. Fragmented REM sleep is also linked with breathing irregularities, which increases the risk of obstructive sleep apnea.
Reduced CPAP Compliance
Veterans with PTSD may find continuous positive airway pressure (CPAP) therapy difficult due to claustrophobia or discomfort, which exacerbates untreated sleep apnea.
A study found that veterans with PTSD have only 41% CPAP adherence as compared to 70% of those without, due to issues like nightmares, claustrophobia, and mask discomfort, reducing the effectiveness of the sleep apnea treatment.
Lifestyle Changes
PTSD-related anxiety and depression often cause poor eating habits, disrupted sleep patterns, and sedentary behavior, further increasing the risk of obstructive sleep apnea (OSA).
Research Findings on PTSD and Sleep-Disordered Breathing
Vietnam-Era Twin Veterans Study
Researchers from the National Center for PTSD and VA medical centers studied male Vietnam-era twins to see how PTSD links to sleep apnea using overnight polysomnography (JAMA Network Open, 2024). Veterans with higher PTSD scores had more apnea events, longer periods of low oxygen, and worse sleep quality, even after controlling for weight and heart health. Because twins share genes and upbringing, the findings suggest PTSD itself contributes to OSA severity and highlight the need for targeted screening and treatment.
Meta-analysis of OSA in PTSD Populations
A meta-analysis published in Sleep Medicine gathered results from 12 studies of veterans and civilians with PTSD and found that about 75% of participants had mild OSA and nearly half had moderate OSA. Veterans were particularly affected, and PTSD was linked to significantly poorer CPAP adherence, including fewer nightly hours of use and lower odds of regular use compared to non-PTSD patients. These results show that screening alone is insufficient and that extra support may be needed to improve treatment success.
Younger OEF/OIF/OND Veterans Study
Finally, a study of younger OEF/OIF/OND veterans (J Clin Sleep Med, 2015) examined 195 Iraq and Afghanistan veterans receiving PTSD care. Nearly 70% screened high-risk for OSA, which was far higher than the general population rates. Higher PTSD symptom scores were strongly tied to increased risk for snoring and daytime fatigue. Interestingly, classic OSA risk factors such as older age or high BMI were less common, suggesting PTSD symptoms themselves may directly elevate sleep apnea risk among younger veterans.
How VA Proves Secondary Service Connection for Sleep Apnea Caused by PTSD
Before you file a VA disability claim for sleep apnea secondary to PTSD, understand how the VA decides these cases. Under regulation 38 CFR §3.310, the VA allows secondary service connection when a service-connected condition, such as PTSD, is “proximately due to or the result of” another disability.
That means, VA benefits may be granted if:
- Direct causation – PTSD directly leads to the development of sleep apnea.
- Aggravation – PTSD doesn’t cause sleep apnea, but makes it permanently worse beyond normal progression.
The “Aggravation” Rule (§3.310(b))
If your PTSD makes your sleep apnea worse over time (not just temporary flare-ups), the VA can still grant secondary service connection under 38 C.F.R. § 3.310(b), but only for the extra disability caused by PTSD. In other words, the VA subtracts your pre-aggravation baseline from your current severity to figure out the portion linked to PTSD.
Because the VA relies heavily on clear medical reasoning to confirm these links, a well-written nexus letter from a qualified provider can be essential evidence that connects your PTSD symptoms to your sleep apnea.
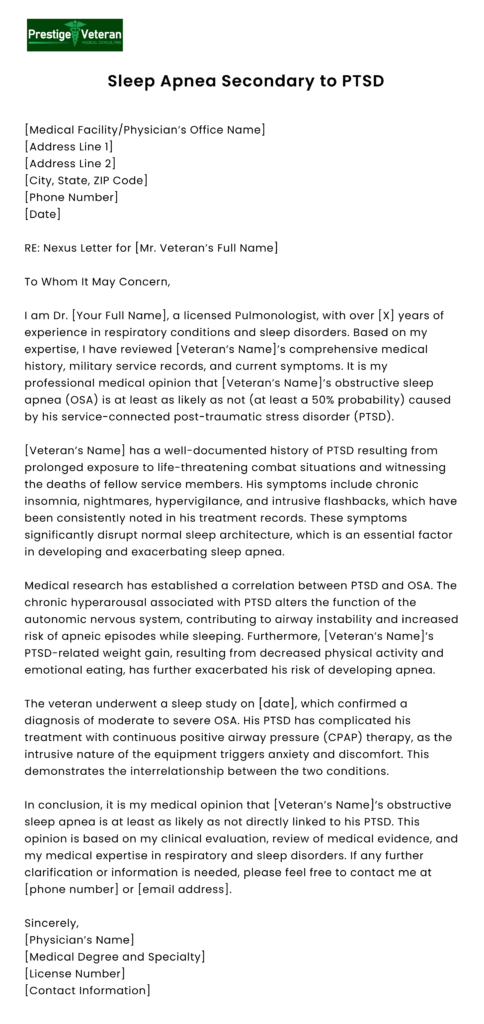
What Is a Nexus Letter for Sleep Apnea Secondary to PTSD? And Why Is it Important?
A nexus letter for sleep apnea secondary to PTSD is a crucial document written by a licensed medical professional. This medical opinion aims to demonstrate that the primary condition has either caused or worsened the veteran’s secondary condition.
While the VA does not mandate a nexus letter for secondary service connection, it is often helpful for claims where a sleep disorder was not diagnosed during service or lacks a direct military connection.
To strengthen your VA disability claim, a nexus letter for sleep apnea secondary to PTSD should include:
- Provider’s Credentials: Written and signed by a licensed medical professional (e.g., M.D., specialist in respiratory conditions, or pulmonologist) with expertise in VA claims. Their qualifications, specialty, and experience should be outlined.
- A Formal Diagnosis: Confirmed through a sleep study.
- Service-Connected PTSD: A documented PTSD diagnosis with an existing VA rating.
- Strong Nexus Opinion: States it is “at least as likely as not” that PTSD caused or aggravated the apnea.
- Evidence-Based Rationale: References peer-reviewed studies, clinical findings, or service records supporting the link.
- Comprehensive Medical Review: Includes sleeping test results, PTSD history, and military and post-service medical records.
- Clear Explanation: Describes how PTSD symptoms, such as chronic stress, nightmares, or medication side effects, contribute to apnea.
By providing expert analysis and supporting evidence, a nexus letter is often vital in proving a link for secondary service connection between PTSD and sleep apnea, helping veterans receive the VA ratings and compensation they deserve.
Sleep Apnea Secondary to PTSD Nexus Letter Example
This nexus letter example aims to establish a clear medical link between a veteran’s service-connected PTSD and the onset and progression of OSA.
VA Ratings for Sleep Apnea Secondary to PTSD
According to 38 CFR § 4.97 – Respiratory System, the VA rates sleep apnea under Diagnostic Code 6847, and the severity of your symptoms helps determine the percentage rating. Here’s how the sleep apnea rating breaks down:
| VA Rating | Criteria |
| 0% | Diagnosed sleep apnea with no symptoms that require treatment. |
| 30% | Persistent daytime hypersomnolence (excessive sleepiness). |
| 50% | Requires the use of a CPAP machine or other breathing device. |
| 100% | Chronic respiratory failure with carbon dioxide retention, cor pulmonale, or requires tracheostomy. |
The 50% rating is the most common for sleep apnea secondary to post-traumatic stress disorder, as veterans often require a CPAP machine.
VA Ratings for PTSD and How They Affect Your Claim
Because PTSD is usually the “primary” service-connected condition when claiming sleep apnea secondarily, understanding its VA rating can help you estimate your combined disability percentage. The VA evaluates PTSD under the General Rating Formula for Mental Disorders (38 CFR §4.130, Diagnostic Code 9411) with possible ratings of 0%, 10%, 30%, 50%, 70%, or 100%, depending on symptom severity and occupational and social impairment.
Criteria for VA PTSD ratings include:
- 0% – Diagnosed, but symptoms don’t impair work/social life or need medication.
- 10% – Mild/transient symptoms during stress or controlled by meds.
- 30% – Occasional work efficiency decreases; depressed mood, anxiety, sleep issues, mild memory loss.
- 50% – Reduced reliability/productivity; frequent panic, impaired thinking/judgment, relationship problems.
- 70% – Deficiencies in most areas; suicidal ideation, near-continuous panic/depression, impaired impulse control, neglect of hygiene.
- 100% – Total occupational/social impairment; delusions, severe memory loss, grossly inappropriate behavior, danger to self/others, disorientation, unable to perform daily living.
A higher PTSD rating can increase your overall combined disability percentage when sleep apnea is added as a secondary condition.
Combined VA Disability Ratings
If you are already service-connected for PTSD, which often carries a rating of 70%, a 50% sleep apnea rating can significantly increase your combined disability rating. This increase can lead to higher monthly compensation and eligibility for Total Disability Individual Unemployability (TDIU) benefits.
Proposed (Not Final) Sleep Apnea Rating Changes
Status: The VA has proposed revising ratings for respiratory conditions, including sleep apnea, under Diagnostic Code (DC) 6847. These proposals, introduced through a 2022 Notice of Proposed Rulemaking and updated in a September 12, 2024, Supplemental Proposed Rule, will not take effect until a Final Rule appears in the Federal Register.
Track the rulemaking docket (VA-2022-VBA-0009) at Regulations.gov for verified updates.
Under the new system, the VA is set to eliminate the 30% rating and will no longer grant a 50% rating automatically for CPAP use. Instead, ratings will be based on treatment effectiveness, tolerability, and functional impact, including end-organ damage:
- 100%: Sleep apnea with end‑organ damage, due to ineffective or unusable treatment.
- 50%: Treatment is ineffective or unusable without end‑organ damage.
- 10%: Incomplete symptom relief despite treatment.
- 0%: Asymptomatic, regardless of treatment status.
That means, veterans whose symptoms are well‑controlled with CPAP may only qualify for a 10% rating even if treatment is effective.
Until any new regulations are officially implemented, the current criteria under DC 6847 remain in place.
For a detailed breakdown of these proposed changes and guidance on how to protect your benefits, read our blog on VA Sleep Apnea Rating Changes in 2025.
What is VA’s “Intermediate Step” Rule?
Many veterans don’t realize that obesity can serve as an “intermediate step” in connecting PTSD to obstructive sleep apnea (OSA) in VA disability claims. Although the VA does not recognize obesity as a standalone service-connected condition, it can be used as a linking factor in establishing secondary service connection under 38 CFR § 3.310.
For instance, if PTSD causes significant weight gain, due to medication side effects, inactivity, or emotional eating, and that obesity leads to or aggravates sleep apnea, this chain of causation can form the basis of an approved claim.
Evidence for a Strong Claim:
- Medically link PTSD to weight gain/obesity
- Prove obesity aggravated or caused OSA
- A nexus letter from a medical professional explaining the chain of causation—PTSD → Obesity → Sleep Apnea
- Cite VA’s Precedent Opinion VAOPGCPREC 1-2017, stating that obesity can be considered an “intermediate step” in establishing secondary service connection
- Use medical studies showing PTSD’s link to metabolic issues
This intermediate step rule allows veterans to seek full recognition of their interconnected health issues.
Steps to Prove Sleep Apnea Is Secondary to PTSD
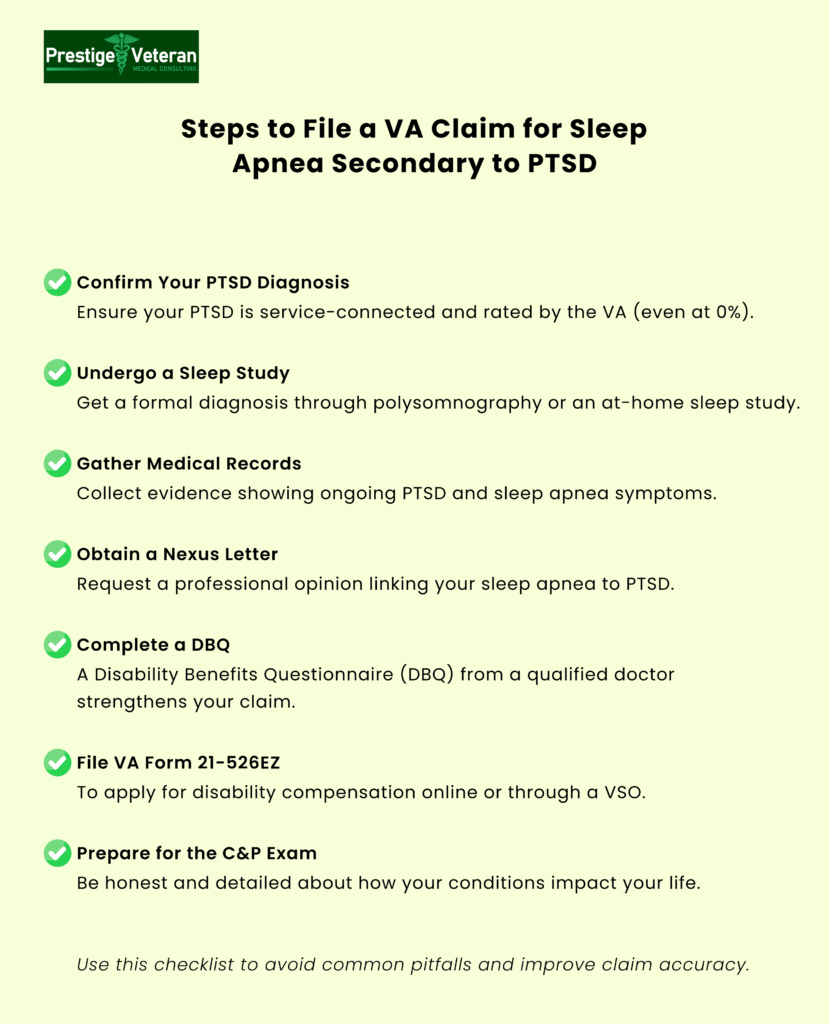
1. Obtain a Sleep Apnea Diagnosis
Typically, the first essential step is to undergo a formal sleep study, also known as polysomnography, without which your VA disability claim cannot move forward. Polysomnography evaluates breathing patterns, heart rate, and oxygen levels, either in a sleep lab or through a home-based test.
2. Establish Service-Connected PTSD
For a secondary claim for sleep apnea, having an established service connection for PTSD is an important factor. PTSD acts as the “primary” condition, providing the basis for linking sleep apnea as a secondary condition. Even a 0% PTSD rating can support this connection, as it demonstrates a recognized mental health impact that could contribute to or aggravate the VA disability.
3. Find a Qualified Medical Professional
To write a nexus letter that links your sleep apnea to your service-connected PTSD, look for a medical expert specializing in sleep disorders, psychiatry, or veterans’ disability claims. You can even request a primary care physician, pulmonologist, or any mental health professional. Providers who understand VA nexus requirements will write stronger letters. Your treating provider or your VA healthcare provider may be willing to assist.
4. Request a Comprehensive Nexus Letter
For veterans obtaining these reports, the nexus letter should include a detailed medical opinion clearly explaining how PTSD contributes to or aggravates sleep apnea. The strongest nexus letters reference specific symptoms of PTSD, such as chronic hyperarousal, anxiety, or insomnia, that potentially lead to apneic episodes. Sound reports include supporting medical literature or studies linking both conditions to strengthen your claim.
5. Supporting Evidence
Each piece of supporting evidence may strengthen a VA claim for sleep apnea secondary to PTSD:
- Medical records showing treatment for PTSD and sleep apnea.
- Results from your polysomnography.
- Lay statements from loved ones or fellow service members who can describe observed symptoms.
- VA treatment notes documenting overlapping issues like insomnia or breathing difficulties.
- Medical research studies highlighting how PTSD exacerbates the risk of sleep-disordered breathing.
- Complete a Sleep Apnea Disability Benefits Questionnaire (DBQ)
Submitting a DBQ and Nexus Letter Together
A completed Disability Benefits Questionnaire (DBQ) for sleep apnea offers the VA detailed insights into the condition, including the severity of PTSD symptoms, treatments such as CPAP usage, and the functional impact on daily life. When completed by a qualified physician, the DBQ provides essential information for determining an appropriate disability rating.
- Combining the DBQ with a nexus letter presents the adjudicators with a comprehensive view of the relationship between conditions, potentially eliminating the need for a C&P exam.
- If your VA claim has been denied, this evidence combination can help you with Supplemental Claims.
It is important to remember that DBQ documents can be provided at little to no cost at the VA C&P exam or by your treating provider if they are willing to assist.
C&P Exam for Sleep Apnea Secondary to PTSD
The Compensation and Pension (C&P) exam primarily verifies whether your sleep apnea was either caused or worsened by your service-connected PTSD. Veterans must attend this examination as it affects the final VA rating and compensation for their disability claim.
How to Prepare and Succeed:
- Review Your Medical Records Thoroughly
Know your sleep apnea diagnosis and ensure a completed sleep study is in your file. Look for any mention of sleep disturbances or fatigue that occurred after PTSD onset. - Understand What the VA Looks For
The VA examiner evaluates:- PTSD diagnosis and severity
- Sleep apnea confirmed by a sleep study
- A “nexus” or logical link between the two, possibly supported by an Independent Medical Opinion (IMO)
- Highlight Indirect Connections
Weight gain due to PTSD-related medications, emotional eating, or reduced physical activity can strengthen your claim. - Prepare for Specific Questions
Be ready to answer questions on your medical history, sleep apnea and PTSD symptoms, impact on daily functioning, and ongoing treatments, including CPAP therapy. - Detail Daily Impact
Share stories that reflect how both service-connected disabilities impair your work, relationships, or daily tasks. Open about your hardest days, mentioning symptoms like exhaustion, anxiety, claustrophobia with CPAP, or frequent nighttime awakenings.
Being detailed, honest, and medically prepared can significantly increase your chances of a favorable outcome in a C&P exam for sleep apnea secondary to PTSD.
VA’s Duty to Assist and Evidence Standards
Under 38 CFR §3.159, the VA has a legal duty to help you develop your disability claim. They assist you by:
- Telling you what evidence is needed to prove your claim.
- Requesting relevant records from federal agencies (e.g., VA hospitals, DoD).
- Helping you obtain private medical records when you authorize it.
- Providing a VA medical examination or nexus opinion when necessary.
However, veterans are responsible for submitting enough evidence for the VA to decide their secondary claims.
4 Reasons Why VA Denies Sleep Apnea Secondary to PTSD Claims
Lack of a Formal Sleep Study
One of the primary reasons for VA denials of sleep apnea secondary to PTSD claims is the absence of a documented sleep study or diagnosis. Without this, the VA is unlikely to recognize this condition as a legitimate condition, let alone approve it as service-connected. A formal sleep study provides essential medical documentation.
Missing Nexus or Link
A contributing reason behind sleep apnea secondary to PTSD denied claim is not including a well-supported nexus letter. The VA requires a strong medical rationale explaining how your PTSD caused or aggravated sleep apnea, especially if there was no diagnosis during service.
That is why a nexus statement from your treating provider or the VA C&P examiner is helpful, even though it is not mandatory. Moreover, symptoms such as chronic hyperarousal, disrupted sleep architecture, or medication side effects must be addressed in VA disability nexus letters to establish a credible, secondary service connection.
Insufficient Medical Evidence
Insufficient medical evidence is a common reason for VA claim denials. Strengthening a secondary service connection for sleep apnea often involves providing comprehensive documentation, including but not limited to the following, when applicable:
- Polysomnography results
- A nexus letter
- Military medical records
- Buddy statements
- A completed Disability Benefits Questionnaire (DBQ) for sleep apnea from a qualified physician
Failure to Connect Obesity to PTSD
Sleep apnea claims secondary to PTSD often face denials because veterans fail to demonstrate weight gain as a result of PTSD symptoms. Many claims are denied because the VA attributes sleep apnea solely to obesity, without a clear connection to the service-connected PTSD.
Under the VA’s “intermediate step” theory, veterans must show that PTSD caused significant weight gain due to factors like medication side effects, emotional eating, or reduced physical activity, which then led to OSA. Without medical evidence linking PTSD to obesity and, in turn, to sleep apnea, the VA often rejects the claim despite its legal and medical validity.
If you have already been denied, consider filing a Higher-Level Review or Supplemental Claim with new, stronger evidence.
Other Conditions Secondary to Sleep Apnea
Sleep apnea, a common service-connected condition among veterans, often contributes to additional health issues that can be claimed as secondary disabilities. Aside from PTSD, veterans may experience significant comorbidities linked to the condition that maximize VA disability ratings and compensation.
- Hypertension – Interrupted breathing raises blood pressure, straining the heart.
- Heart Disease – Low oxygen during sleep can worsen atrial fibrillation or heart failure.
- Diabetes – Poor sleep disrupts glucose metabolism, increasing Type 2 diabetes risk.
- Chronic Fatigue & Migraines – Poor sleep quality impacts daily function.
- Depression & Anxiety – Sleep deprivation worsens mental health beyond PTSD.
- GERD – Interrupted REM sleep or CPAP use can trigger acid reflux.
- Obesity – This is both a cause and effect of sleep apnea, creating a cycle that worsens symptoms.
Veterans experiencing these secondary conditions should document clear medical evidence connecting them to their sleep apnea.
Real BVA Case Examples: Veterans Who Won Their Sleep Apnea Claims
A powerful step in strengthening your claim is to reference favorable Board of Veterans’ Appeals (BVA) decisions that have granted service connection for sleep apnea secondary to PTSD. In multiple notable cases, the BVA sided with independent private medical opinions over VA examiners, especially when those opinions were backed by peer-reviewed medical studies and reasoning that linked PTSD to sleep-disordered breathing. For example,
BVA Decision 1
In one appeal, a Vietnam-era veteran won a landmark Board decision granting service connection for obstructive sleep apnea secondary to PTSD, awarding TDIU retroactive to November 7, 2016, and increasing the PTSD rating to 100 percent effective July 28, 2020.
The ruling highlighted evidence including:
- A 2019 private Disability Benefits Questionnaire (DBQ).
- A medical opinion from a private physician that cited research linking PTSD, sedating medications, and increased risk of obstructive sleep apnea.
This evidence outweighed an earlier 2018 VA negative opinion and established the required nexus. The Board also remanded Special Monthly Compensation under 38 U.S.C. §1114(s) for rating assignment of the newly service-connected sleep apnea.
Citation Nr. 21016778, Docket No. 19-24 609 (Bd. Vet. App. Mar. 23, 2021).
BVA Decision 2
In another decision, the Board of Veterans’ Appeals granted secondary service connection for obstructive sleep apnea (OSA) linked to service-connected PTSD, because,
- The veteran’s OSA was confirmed by a sleep study and supported by prior diagnoses of upper airway resistance syndrome and ongoing PTSD symptoms.
- A 2013 VA psychiatrist’s opinion, referencing research showing higher OSA rates in combat veterans with PTSD, provided a strong medical nexus.
This favorable opinion outweighed less-definitive opposing evidence. The Board determined that PTSD directly contributed to the precursor airway condition that later developed into OSA, satisfying the medical nexus requirement and establishing full secondary service connection.
Citation Nr. 1316035, Docket No. 08-00309 (Bd. Vet. App. May 15, 2013)
Hence, these BVA decisions underscore the importance of credible nexus opinions, medical literature, and documented symptom history in VA disability claims.
Nexus Letter Cost and How to Find a Qualified Writer
A well-crafted nexus letter for sleep apnea secondary to PTSD can be the difference between a denied and approved VA claim. But how much does it cost, and where do you find a qualified provider?
Cost:
Nexus letter prices are on average $1200, depending on the medical provider’s experience, credentials, and the complexity of your case. Some may offer military discounts or sliding-scale pricing.
Where to Find a Nexus Letter Provider:
- Private Medical Professionals – Pulmonologists, psychiatrists, and internists experienced in VA claims can write nexus letters, though availability may be limited.
- Specialized Nexus Letter Providers – Trusted providers like Prestige Veteran offer a fully VA‑compliant Independent Medical Opinion (IMO) written by experienced medical professionals who understand VA claim standards and terminology.
- Telehealth and Online Medical Services – Some virtual clinics offer nexus letters, but be cautious to ensure they meet VA evidence standards.
- Veteran Service Organizations (VSOs) – While VSOs don’t write nexus letters, they may help refer you to reputable providers.
- Your VA or Civilian Doctor – If your treating physician is familiar with VA guidelines and willing to support your claim, they may be able to write a statement or full nexus opinion.
Tip: Always choose someone with VA claims experience and ensure they use language like “at least as likely as not” in a nexus letter linking PTSD to your service-connected sleep apnea.
Professional Assistance and Guidance
Secondary service connection claims can be complex, and professional assistance ensures your case is as strong as possible. Consider consulting VA-accredited attorneys, claims agents, or veteran service organizations (VSOs) to guide you through the process. These experts provide legal advice, can assist with sleep apnea nexus letters, and advocate for your rights to secure proper compensation.
Conclusion
Establishing a connection between PTSD and sleep apnea is an important step for veterans seeking VA disability benefits for these related conditions. A well-crafted VA nexus letter, backed by solid medical evidence, can greatly enhance the chances of a successful claim in some cases. With consistent documentation and expert support, veterans can build a strong case that improves their chances of getting the benefits they have earned through their military service.
FAQs
What is the nexus between sleep apnea and PTSD?
The nexus lies in their bidirectional relationship, where PTSD-related stress, hyperarousal, and disrupted rest increase sleep apnea risk, while untreated sleep apnea worsens PTSD symptoms, creating a vicious cycle.
Can I claim sleep apnea secondary to PTSD?
Yes, you can claim. Submit a formal diagnosis, medical evidence, and a medical nexus letter stating that your service-connected PTSD either caused or aggravated your sleep apnea.
What is a nexus letter for sleep apnea related to PTSD?
A nexus letter is a written medical opinion from a qualified healthcare provider that explains how your PTSD likely caused or worsened your sleep apnea, often using the phrase “at least as likely as not” to meet VA standards for service connection.
How to write a successful VA claim for sleep apnea secondary to PTSD?
You need documentation of:
- A confirmed sleep apnea diagnosis via a sleep study
- Established service-connected post-traumatic stress disorder
- A detailed nexus letter from a qualified medical professional
- Supporting evidence such as sleep studies, medical records, and a completed DBQ
What is the sleep apnea secondary to PTSD VA rating?
Sleep apnea secondary to PTSD is typically rated at 50% if a CPAP machine is required, but can be 0%, 30%, 50%, or 100% depending on symptom severity. Although the 2025 proposed rule changes may revoke the automatic 50% for CPAP use, making the rating dependent on treatment effectiveness or intolerance.
What is a C&P exam for sleep apnea secondary to PTSD?
A Compensation and Pension (C&P) exam is a VA medical evaluation that assesses the severity of sleep apnea, its link to PTSD, and its impact on the veteran’s daily functioning and overall health.
How to prove sleep apnea secondary to PTSD in a C&P exam?
Bring your sleep study results, CPAP usage data, supporting documentation like nexus letters linking your PTSD to your sleep apnea, and be ready to explain how both conditions affect your daily life.
How to win a sleep apnea VA claim?
Get a confirmed sleep study diagnosis, show a direct service connection or link to PTSD, and back it with lay statements and a strong medical nexus letter. Ensure you describe your symptoms and daily life impact thoroughly during the C&P exam.
What is sleep apnea, a secondary condition of?
Sleep apnea is most often claimed as secondary to PTSD, but can also be linked to PTSD, obesity, tinnitus, nasal or sinus problems, or other service-connected disorders that affect breathing or sleep.
Can a psychiatrist write my nexus letter for this case?
Yes, a psychiatrist can write a nexus letter for sleep apnea if they can provide a credible medical opinion linking the condition to service-connected PTSD, meeting VA standards.
How long will it take to reverse damage from sleep apnea?
Damage from untreated sleep apnea can improve within weeks to months after consistent treatment like CPAP, but full reversal depends on severity and how long it’s been untreated.
Also read: The Role of a Nexus Letter for Obstructive Sleep Apnea (OSA) Claims
At Prestige Veteran Medical Consulting, a veteran-owned company, we specialize in Independent Medical Opinions (IMOs) known as Nexus letters.
Our purpose is to empower YOU, the veteran, to take charge of your medical evidence and provide you with valuable educational tools and research to guide you on your journey.
Understanding the unique challenges veterans face, our commitment lies in delivering exceptional service and support.
Leveraging an extensive network of licensed independent medical professionals, all well-versed in the medical professional aspects of the VA claims process, we review the necessary medical evidence to incorporate in our reports related to your VA Disability Claim.
Prestige Veteran Medical Consulting is not a law firm, accredited claims agent, or affiliated with the Veterans Administration or Veterans Services Organizations. However, we are happy to discuss your case with your accredited VA legal professional.














One Response