As a veteran, reading a decision letter that says your condition isn’t linked to service can be tough, especially when your symptoms are real and deeply tied to your experiences in uniform. The Department of Veteran Affairs (VA) reported that around 36 percent of disability claims were initially denied in fiscal year 2024, showing how common these frustrations are.
Even highly credible veterans are denied benefits because the evidence wasn’t presented clearly enough. In this blog, we explain what the VA requires to establish a service connection, why claims are often denied, and the steps you can take to strengthen your case for approved benefits.
Table of Contents
What “Not Service Connected” Really Means
When the VA says a condition is “not service connected,” it simply means the VA does not believe your disability was caused or aggravated by your military service. It does not mean you are not disabled, only that the VA has not found enough evidence to link your condition to your time in uniform.
What “Service Connected” Means
A service-connected disability is any illness, injury, or condition that began during active duty, was caused by service, or was made worse by service, as defined in 38 C.F.R. § 3.303. When the VA grants service connection, the veteran can become eligible for disability compensation, health care, and other benefits.
How to Get a Condition Service Connected
To qualify for VA disability compensation, a veteran must establish a service connection, which requires proving three key elements:
- A current medical diagnosis from a qualified provider
- Evidence of an in-service event, illness, injury, or exposure
- A medical nexus stating the condition is “at least as likely as not” related to service
If any of these elements are missing, unclear, or not supported by strong evidence, the VA may deny the claim and state the condition is not service connected.
The Burden of Proof Is Lower Than Most Veterans Think
To grant service connection, the VA only needs evidence showing the disability is:
“At least as likely as not”
(meaning 50/50 probability)
This standard, established under the VA’s Benefit of the Doubt rule, exists to favor the veteran when the evidence is evenly balanced, not to block them. But if the VA rater does not see medical or factual evidence meeting that threshold, the claim gets denied. Let’s discover the main reasons why your condition might not get service-connected.
Why VA Claims Get Denied for Lack of Service Connection
A denial labeled “not service connected” is one of the most common outcomes veterans face when filing for disability benefits. Even when diagnoses are clear and symptoms are debilitating, the VA requires specific types of evidence to establish the legal link between a veteran’s disability and their military service. Understanding the most frequent reasons for VA denials helps veterans know what evidence may be missing and how to correct it.
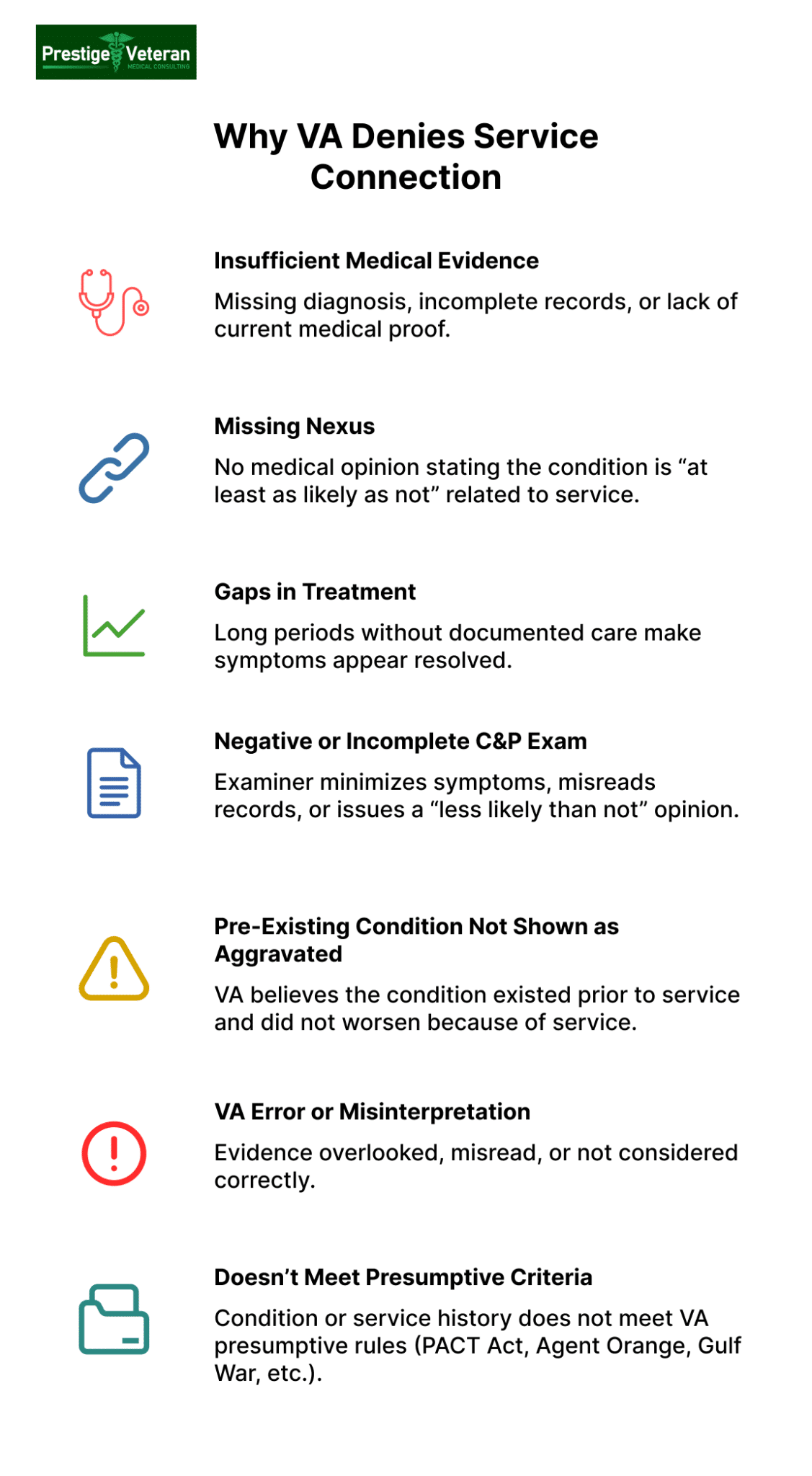
1. Insufficient Medical Evidence
One of the top reasons veterans receive a “not service-connected” decision is a lack of current medical diagnosis and its relationship to service, even when symptoms are obvious. You may not qualify for VA disability compensation if you haven’t submitted or demonstrated elements like:
- A current diagnosis
- Treatment records showing onset and progression of symptoms during and after service
- Medical evidence showing the condition is still active
A current, well-documented diagnosis missing from your records can sometimes even result in the VA denying the claim before even scheduling a C&P exam.
2. Weak or Missing Nexus (“Link”)
Even with a solid diagnosis, your VA disability claim can get denied if there’s no medical nexus letter or opinion explaining why the condition is “at least as likely as not” related to service. When examiners cannot find a logical connection between military events and the disability, especially for conditions diagnosed years or decades after separation, the VA rater is generally required by law to deny service connection.
Moreover, if a provider fails to use VA-approved language or gives a speculative opinion (for example, the veteran’s back pain “may be related to service”), the VA will often disregard the nexus letter.
3. Gaps in Treatment or Lack of Continuity
Continuity of symptoms is a key requirement in proving service connection for VA disability, especially for musculoskeletal, mental health, and chronic pain conditions. It’s because inconsistent treatment often leads the VA to assume that symptoms got resolved long before the filed claim. The VA can, at times, deny a claim when it sees:
- No medical visits after service
- Large gaps in treatment
- Little or no evidence of ongoing, chronic symptoms
For example, a veteran’s records show an in-service injury and a diagnosis today, but no documented follow-up treatment in between, the VA may conclude the disability resulted from age, lifestyle, or a post-service incident rather than military service.
4. Incomplete or Negative C&P Exam Findings
The Compensation & Pension (C&P) exam often carries significant weight in the VA’s decision-making process. Many veterans experiencing a favorable C&P exam may still have their VA disability denied if the examiner:
- Fails to thoroughly review or misinterprets your records
- Minimizes symptoms or functional impact
- States the condition is “less likely than not” related to service
- Conducts a rushed or incomplete exam
Many veterans overturn these decisions by considering options like obtaining an independent medical opinion to challenge the unfavorable exam or identifying errors through a Higher-Level Review.
5. Pre-existing Conditions the VA Believes Were Not Aggravated
If the VA believes your condition existed before service and did not worsen due to service, the claim is often denied. Under 38 CFR §3.306, aggravation requires showing that the underlying condition worsened beyond natural progression.
For example, a veteran with childhood asthma who later deployed to burn-pit environments must show medical evidence demonstrating chronic worsening. An expert medical opinion explaining why service-related exposures aggravated the pre-existing condition can be pivotal to overturning this type of denial.
6. Misinterpretation of Evidence or VA Error
Unfortunately, human error happens. Records are overlooked, evidence is misread, and favorable facts may not be considered. This is where appeal options like Higher-Level Review often help resolve mistakes, especially in cases where a VA-accredited legal professional is involved.
7. When Presumptive Service Connection Doesn’t Apply
Many veterans believe their condition should qualify as PACT Act presumptive. However, each presumptive category, such as Agent Orange Exposure, Gulf War Illness, or Burn Pits, has strict eligibility rules. If a veteran’s service location, time period, or medical diagnosis does not meet VA presumptive criteria, their claim may be denied for lack of service connection without a traditional nexus letter.
See the full list of PACT Act VA presumptive conditions.
What to Do If Your VA Claim Is Denied
Once you understand why the claim denial occurred, the next step is selecting the right appeal lane. Here are the three options under the Appeals Modernization Act (AMA):
1. Request a Higher-Level Review (HLR)
A Higher-Level Review (VA Form 20-0996) is ideal when the VA overlooks favorable findings or misinterprets critical evidence documenting an in-service event. In an HLR, a more experienced VA reviewer re-examines your claim with the same evidence for legal or factual mistakes.
2. File a Supplemental Claim
A Supplemental Claim (VA Form 20-0995) may be considered when you have new and relevant evidence linking the condition to service, which the VA claimed was missing or incomplete.
Example: A veteran denied service connection for knee arthritis later submits a private orthopedist’s nexus letter linking the condition to repeated infantry training. The new nexus evidence submitted via a supplemental claim can lead to approval.
3. Appeal to the Board of Veterans’ Appeals (BVA)
A Board Appeal is often ideal when a denial involves complex disabilities, repeated findings of “not service connected”, or situations requiring expert testimony. Veterans may submit new evidence or request a hearing before a Veterans Law Judge to clarify how the condition began in service or was aggravated by it.
Note: Reapplying instead of appealing can alter or impact an earlier effective date and cost years of potential back pay in some circumstances. Always consider filing an appeal or supplemental claim with the assistance of an accredited legal professional before starting over. Learn more about your appeal options on the VA’s official page: Decision Review and Appeals.
How to Prove Your Disability Is Service Connected
Fortunately, service-connection denials are among the most reversible decisions when the right medical and factual evidence is added. Strengthening your claim involves correcting the gaps the VA identified and presenting evidence in a clear, regulation-based format.
Step 1: Read Your VA Rating Decision Carefully
Begin by examining the VA Rating Decision carefully so you understand why your claim was denied. Focus on the “Evidence Reviewed,” “Reasons for Decision,” and any favorable findings. These sections reveal what evidence was considered and where the VA found gaps, such as missing medical documentation or a lack of proof of an in-service event. Reviewing your decision letter thoroughly helps you decide what type of evidence must be added.
Step 2: Reinforce the In-Service Event or Exposure
If the VA states that your in-service event was not established, you may consider strengthening the factual record. Many veterans lose out on disability benefits because their service documentation is incomplete or missing. Providing supplementary evidence can show that the military-related injury or exposure actually did occur, such as:
- Service treatment records and personnel files
- Line of duty findings
- Deployment records (including your DD-214)
- Unit histories or training logs
- Buddy statements describing what they witnessed
Reconstructing what caused or aggravated your VA disability is essential for proving its service connection.
Step 3: Strengthen the Nexus with a Qualified Medical Opinion
A nexus letter or independent medical opinion (IMO) is often the deciding factor in overturning a denied service connection into a granted one because it clearly explains how your military service caused or aggravated your condition. This nexus opinion must include VA’s terminology of “at least as likely as not”, supported by pathology, medical literature, and service treatment records when available.
For example, a private provider can establish a secondary service connection with a nexus statement:
“It is my professional medical opinion that the Veteran’s gastroesophageal reflux disease (GERD) is at least as likely as not (50% probability or greater) to have contributed to the onset and progression of the Veteran’s obstructive sleep apnea. This opinion is based on the known physiological relationship between recurrent nighttime reflux, upper airway inflammation, and subsequent airway obstruction.”
Ideally, this nexus letter should come from a qualified healthcare professional familiar with VA disability claims who has reviewed your full medical and service history. Many veterans seek independent medical opinions when VA examiners provide unfavorable conclusions.
Step 4: Demonstrate Continuity of Symptoms After Service
Showing your symptoms continued after discharge is crucial to establishing that the disability never resolved and is connected to your service. This is especially important for chronic VA claims like arthritis, migraines, or mental health disorders. Evidence that can prove an ongoing link between service and your condition includes:
- VA and private treatment records from discharge to present
- Prescription history
- Specialist evaluations or imaging
- Personal logs documenting flare-ups
- Lay statements from family or coworkers who observed ongoing problems in function or behavior
- Employment records showing missed work or accommodations
A consistent pattern of symptoms over the years supports the argument that the present disability did not develop on its own, but evolved from an in-service injury or exposure.
Step 5: Use a Sworn Declaration
A Sworn Declaration can at times carry more credibility than an informal personal statement because it is made under penalty of perjury. When records are missing, use this declaration to explain undocumented injuries, timeline of symptoms, or barriers to obtaining medical care during service.
For example, a veteran who injured a shoulder during field exercises can detail the date, conditions, immediate pain, and how the injury affected performance afterward. This legally binding statement may help veterans succeed in appeals by addressing a not service-connected finding.
Step 6: Add Buddy or Lay Statements
Lay evidence helps confirm events or symptoms that military records fail to document. These statements should describe what happened in service, changes in your condition after the event, and the life impact of ongoing symptoms. For example, a squadmate recalling your severe headaches after a barracks accident can help support a traumatic brain injury claim. When the VA doubts the event occurred, reliable statements from service members, supervisors, or friends can verify the condition is service-connected.
Download here: VA Form 21-4138 (Statement in Support of Claim)
Step 7: Challenge an Unfavorable C&P Exam
If your service connection denial relied on a flawed C&P exam, you have the right to dispute the report. Challenge the errors by submitting a written rebuttal and medical evidence that contradicts the examiner’s findings. For example, if a C&P examiner dismisses your knee instability but imaging confirms ligament damage, it will strengthen your argument for service connection and support an appeal.
If you need support, Veterans Service Organizations (VSOs) or representatives can provide free assistance with your claim. Working with a VA-accredited attorney is especially helpful if you are dealing with complex appeals.
Case Study: How a Veteran Reversed a VA Decision
A 54-year-old Army infantry veteran initially received a “Not Service Connected” decision for chronic migraines and PTSD despite documented deployment stressors. His first claim lacked a strong medical nexus, and the VA attributed his symptoms to “post-service stress”. He struggled with recurring migraine episodes, photophobia, and occasional panic attacks triggered by crowds or loud noises, issues that frequently caused job instability and, at times, ER visits.
After the denial, he requested a Higher-Level Review, but the decision was upheld. With representation from a VA-accredited attorney, he decided to pursue a Board of Veterans’ Appeals appeal and gathered stronger nexus opinions by a new VA neurologist and a licensed trauma psychologist. He also secured lay statements from his spouse and platoon sergeant confirming in-service blast exposure and the onset of headaches during deployment, as well as his gradual behavioral changes after returning home.
How the denial was overturned:
- New, detailed medical nexus letter connecting migraines to blast overpressure events
- Updated PTSD diagnosis using DSM-5 criteria tied to documented convoy incidents
- Consistent treatment records showing migraine frequency over 12 days monthly
- Lay statements confirming in-service symptoms and progression after discharge
- Clarifications from a C&P examiner noting functional loss and occupational impairment
The Board of Veterans’ Appeals found the new and material evidence sufficient to overturn the prior denial. The veteran was ultimately granted service connection for chronic migraines and PTSD.
Conclusion
Receiving a claim decision stating your condition is not linked to service doesn’t mean your fight for the VA benefits is over. With the right evidence, professional medical opinions, and a clear understanding of what the VA looks for, many veterans successfully overturn these decisions. The key is knowing where the gaps are and taking strategic steps to address them. Whether you pursue a review or file an appeal, each path offers a chance to reinforce the service connection the VA may have overlooked. Supported by well-documented evidence and professional guidance, you can prove your disability claim and secure the benefits you rightfully deserve.
Frequently Asked Questions (FAQs)
How do I prove my VA disability is service-connected?
You prove service connection by showing things like a current diagnosis, evidence of an in-service event or exposure, and a medical nexus stating your condition is “at least as likely as not” related to service.
Why does my VA claim say not service connected?
A service connection is usually denied because:
- No confirmed medical diagnosis
- No verified in-service event, injury, or exposure
- Weak or missing nexus opinion
- Gaps in treatment or a lack of continuity of symptoms
- Unfavorable or incomplete C&P exam findings
- VA errors or misinterpretation of your records
- Condition does not meet VA presumptive criteria
Can I get VA disability for non-service connected?
You cannot receive VA disability compensation for a non-service-connected condition, but the VA may provide limited health care or pension benefits in certain cases.
My VA claim was denied. Now what should I do?
You can respond to a denial by considering options like filing a Higher-Level Review, submitting a Supplemental Claim with new and relevant evidence, or appealing to the Board of Veterans’ Appeals.
Why did the VA make favorable findings but still deny my claim?
A disability claim can be denied despite favorable findings if the VA believes key evidence, such as a nexus, continuity of symptoms, or proof of an in-service event, is still insufficient to meet service-connection requirements.
Can the VA deny a presumptive disability?
Yes. If the VA decides you do not meet the required service dates, locations, exposures, or diagnosis criteria, they can deny a presumptive condition.
How can I check the status of my VA disability claim?
You can check the status of your VA claim, decision review, or appeal by signing in to the official VA claim status tool on VA.gov or eBenefits. Also read: 10 Mistakes to Avoid in a Medical Nexus Letter
At Prestige Veteran Medical Consulting, a veteran-owned company, we specialize in Independent Medical Opinions (IMOs) known as Nexus letters.
Our purpose is to empower YOU, the veteran, to take charge of your medical evidence and provide you with valuable educational tools and research to guide you on your journey.
Understanding the unique challenges veterans face, our commitment lies in delivering exceptional service and support.
Leveraging an extensive network of licensed independent medical professionals, all well-versed in the medical professional aspects of the VA claims process, we review the necessary medical evidence to incorporate in our reports related to your VA Disability Claim.
Prestige Veteran Medical Consulting is not a law firm, accredited claims agent, or affiliated with the Veterans Administration or Veterans Services Organizations. However, we are happy to discuss your case with your accredited VA legal professional.