For veterans with sleep apnea, Continuous Positive Airway Pressure (CPAP) machines and compliance often raise questions about their impact on VA ratings and disability compensation. Understanding how a CPAP prescription impacts disability benefits can mean the difference between lower and higher monthly compensation. Unfortunately, there is a lot of misinformation that creates confusion, leaving many veterans unsure about what truly matters for their sleep apnea VA claims.
This guide breaks down the myths and facts, helping veterans protect their health while securing the compensation they have earned.
Table of Contents
What is a CPAP and Why Does It Matter for VA Ratings?
A CPAP, or Continuous Positive Airway Pressure machine, is the most common and effective treatment for obstructive sleep apnea (OSA). By delivering a constant flow of air through a mask, it prevents airway collapse during sleep, improves oxygen levels, reduces cardiovascular risks, and restores better rest. Because of its medical importance, the Department of Veterans Affairs (VA) considers CPAP machines “medical devices” when assigning disability ratings.
VA disability ratings for sleep apnea are assigned based on severity and treatment requirements under 38 CFR § 4.97 – respiratory system, Diagnostic Code 6847. The typical breakdown looks like this:
- 0% – Sleep apnea is diagnosed, but symptoms are asymptomatic or controlled without impairment.
- 30% – Evidence of persistent daytime fatigue, hypersomnolence, or functional impact.
- 50% – A CPAP (or similar device) is medically prescribed and required for treatment.
- 100% – Severe cases involving chronic respiratory failure, need for a tracheostomy, or other life-threatening complications.
The reason a CPAP prescription matters so much is that if your doctor determines it is required for treating your condition, it automatically qualifies many veterans for the 50% level, ensuring access to higher monthly compensation. However, compliance matters too. Modern CPAP machines track nightly usage, and VA may review this data to verify consistent treatment. Strong compliance not only improves health but may also bolster a veteran’s disability claim.
But that’s about to change, as the VA is reviewing its criteria for sleep apnea ratings. Veterans should stay informed, since future claims may require stronger medical evidence to prove eligibility.
Proposed VA Sleep Apnea Rating Changes
The Department of Veterans Affairs (VA) is finalizing new rules that will change how sleep apnea is rated, though it is yet to take effect. The new criteria will focus on whether treatment is effective, whether CPAP use is possible, and whether end-organ damage or comorbid conditions are present.
These changes reflect VA’s Feb 15, 2022, proposed rule to update respiratory ratings (including DC 6847) and are not yet final. Monitor the Federal Register docket for updates. 87 Fed. Reg. 8474 (Feb. 15, 2022)
New Sleep Apnea Rating System:
| VA Rating | Criteria |
| 100% | Ineffective treatment + end-organ damage (e.g., heart or lungs) |
| 50% | Ineffective treatment or cannot use CPAP due to comorbid conditions |
| 10% | CPAP treatment offers incomplete relief (per sleep study) |
| 0% | Sleep apnea is asymptomatic, with or without treatment |
Importantly, existing ratings will not be reduced when the new rules take effect. Veterans already rated for sleep apnea will be “grandfathered in” under current laws. According to 38 CFR § 3.105(e), VA cannot reduce a rating without clear evidence of sustained improvement and due process.
Veterans should consider filing before the new rules take effect, as they may secure protections under the current system.
Here’s the full guide on VA Sleep Apnea Ratings: 2025 Proposed Changes
CPAP and VA Ratings: Myths vs. Facts
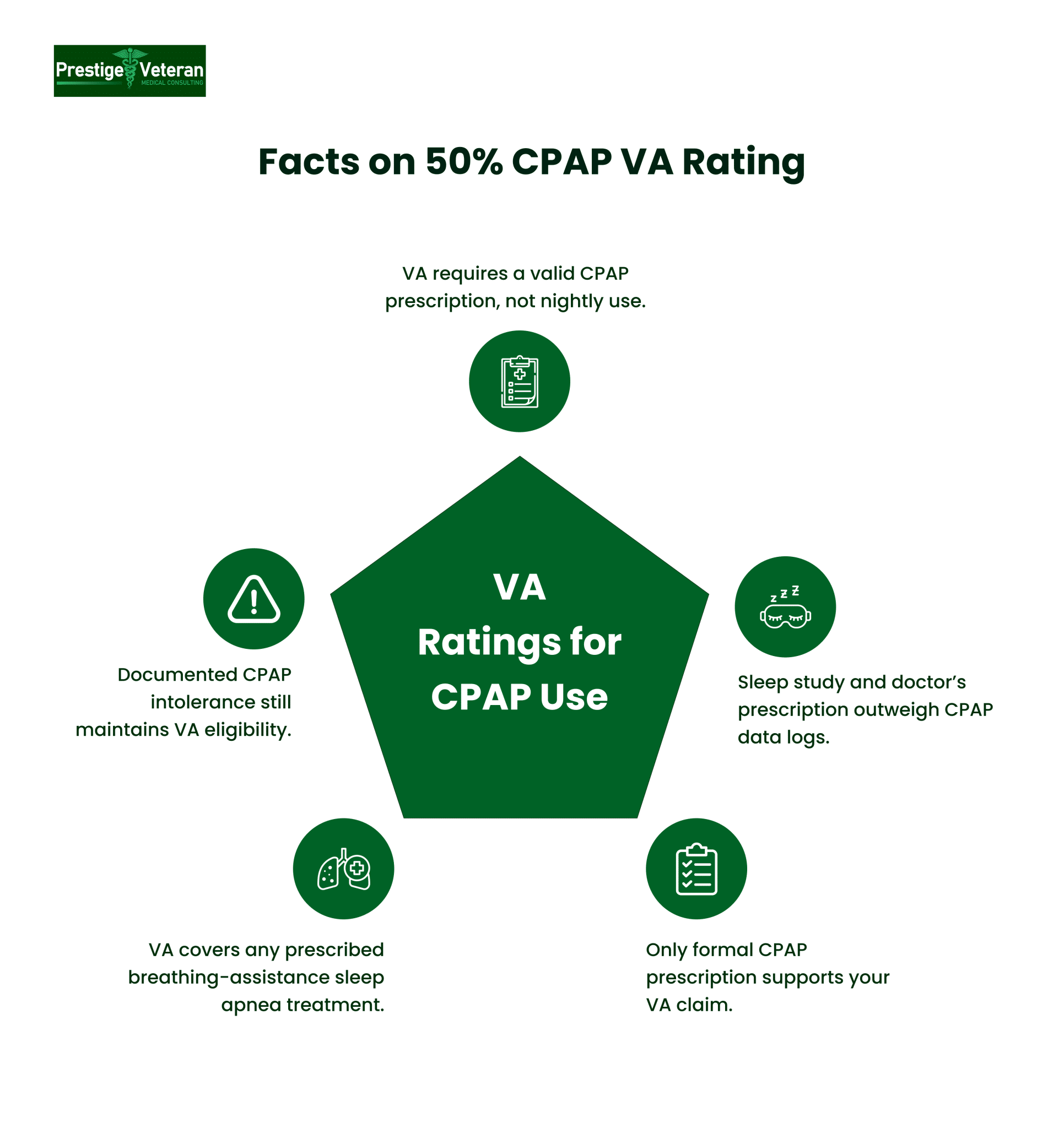
Myth #1: You Must Use Your CPAP Machine Every Night to Qualify for the 50% VA Rating
Fact: The VA does not require you to use your CPAP machine every single night to receive a 50% disability rating for sleep apnea. Under the current Diagnostic Code 6847, the VA bases ratings on whether a Continuous Positive Airway Pressure (CPAP) machine is medically prescribed or recommended, not whether you log perfect compliance.
Even if you struggle with regular use due to comorbidities like claustrophobia, mask discomfort, side effects, or personal circumstances, you may still qualify for benefits. Although daily use of a breathing assistance device is encouraged for your health, it is not a criterion for securing the 50% VA rating.
Myth #2: Downloadable CPAP Data is Required for Your VA Claim
Fact: While many modern CPAP machines transmit usage/download data to healthcare providers or insurance companies, it is not a listed VA requirement for assigning disability ratings. Instead, the key evidence for a 50% rating is a confirmed sleep apnea diagnosis (usually through a sleep study) and a doctor’s prescription for CPAP or other prescribed therapy.
However, compliance data may be reviewed in Compensation and Pension (C&P) exams or re-evaluations as medical evidence of effectiveness, ongoing need, or reasons you cannot tolerate therapy. For an initial claim, VA primarily focuses on medical necessity, not usage metrics.
Myth #3: Even a CPAP Recommendation May Qualify You for Benefits
Fact: Under VA’s schedule (DC 6847), the VA adjudicators require objective medical evidence showing a licensed medical professional prescribed a CPAP or similar breathing device to manage diagnosed sleep apnea, not merely “suggested.”
CPAP Recommended vs. Prescribed
Usually, a recommendation implies the machine hasn’t been formally ordered for treatment, whereas a prescription confirms that a CPAP is medically necessary.
For example, if a sleep study notes “CPAP recommended,” the VA may view it as optional. But if your physician documents “CPAP prescribed for daily management of obstructive sleep apnea,” that formal prescription slip will serve as more concrete medical evidence supporting a higher VA disability rating tied to 50 percent CPAP use.
Veterans seeking benefits should ask their treating physician to convert a recommendation into a formal prescription and state why therapy is required when applicable. Make sure your medical file clearly documents the apnea diagnosis, device prescription, and its ongoing use.
Myth 4: A CPAP Prescription Guarantees a 50% VA Rating Forever
Fact: While a CPAP prescription usually qualifies you for a 50% VA rating for sleep apnea, it’s not guaranteed permanently. The VA may schedule future re-exams to verify if your sleep apnea remains severe enough to need continued treatment.
For example, if your recent sleep study shows improved oxygen levels and your physician notes discontinued CPAP use without a return of symptoms, the VA could lower your rating. To protect your benefits, keep consistent documentation, records of follow-up medical appointments, and ensure your sleep specialist clearly notes your ongoing need for therapy.
Note: Proposed changes in sleep apnea criteria, especially the 50% rating, could impact your VA ratings. Since the new evaluation process is likely to focus on CPAP treatment effectiveness, not just device use, veterans are encouraged to file claims now under the current criteria to help obtain more favorable ratings.
Myth 5: CPAP is the Only Way to Qualify for a Sleep Apnea Rating
Fact: It is true that the Continuous Positive Airway Pressure (CPAP) machine is the most recognized treatment for sleep apnea, but it’s not the only path to VA benefits. Under 38 CFR § 4.97, DC 6847, the VA considers the use of any “breathing assistance device” or treatment prescribed by a doctor to manage sleep apnea, not just CPAP use.
Veterans prescribed alternative sleep apnea treatments can still qualify for compensation, for example:
- BiPAP machines
- Oral appliances (like mandibular advancement devices)
- Supplemental oxygen therapy
- Surgical interventions to remove airway obstructions
If your doctor prescribes medications to manage related issues like excessive daytime sleepiness or insomnia, that evidence can also support your sleep apnea claim. So, if you’re managing obstructive sleep apnea without CPAP, you may still qualify for a VA disability rating.
Myth 6: If You Can’t Tolerate CPAP, You Lose Your Chance at VA Compensation
Fact: Many veterans believe struggles with CPAP, like mask fit, dryness, pressure intolerance, or sleep disruption, jeopardize their VA rating. That’s false. A study by El-Solh et al. (2010) found that veterans with PTSD often have difficulty adhering to CPAP therapy due to nightmares or anxiety. However, this non-compliance does not result in a rating reduction.
VA compensation is based on whether treatment is prescribed, not perfect compliance. If CPAP is intolerable or ineffective, sleep specialists may recommend alternative machines or therapies that still establish medical necessity. Veterans must document challenges to show ongoing management and preserve their eligibility for benefits.
Myth #7: Filing Your Sleep Apnea Claim Anytime Won’t Affect Your VA Rating
Fact: Timing matters. The VA has proposed changes to the sleep apnea ratings, and if they are finalized, the criteria for earning compensation could become stricter. Currently, veterans diagnosed with sleep apnea who require a CPAP machine or other breathing assistance are often awarded a 50% disability rating. Under the proposed rules, that rating may no longer be automatic, and veterans could see lower disability percentages based on CPAP treatment effectiveness and functional impairment.
If you wait to file until after the new standards take effect, you risk losing out on benefits you might qualify for today. Instead, file now to preserve your claim under the current rules and protect your earned compensation.
Why CPAP Compliance Still Matters (Even If It Doesn’t Directly Affect Ratings)
While your VA disability rating for sleep apnea isn’t directly tied to how faithfully you use your CPAP machine, consistent compliance still significantly impacts the outcome of your claim.
According to the Centers for Medicare & Medicaid Services, the minimum compliance requirement is the use of PAP therapy for at least 4 hours per night on 70% of nights during a consecutive 30-day period within the first 90 days of receiving the equipment.
Even though DC 6847 does not require usage data to assign ratings, here are some reasons to comply:
Benefits of CPAP compliance:
- Protects long-term health by lowering risks of serious complications such as heart disease, high blood pressure, stroke, and chronic fatigue.
- Improves sleep quality, leading to deeper rest, better moods, focus, and higher energy levels.
- Prevents daytime fatigue, which can impact safety, productivity, and relationships.
- Strengthens your VA medical record with documented CPAP usage and follow-up visits.
- Supports your VA disability claim if your condition is ever reviewed or re-evaluated, proving the medical necessity of your device.
Even if you struggle with comfort or mask fit, reporting those issues to your doctor helps establish an ongoing need for treatment, ensuring your disability benefits and care remain secure.
What Conditions Qualify as Comorbidities?
When it comes to your VA sleep apnea rating, comorbid conditions can play a decisive role. Under the new rules, ratings are no longer based only on CPAP prescriptions but on whether treatment is effective or even possible. This is where comorbidities matter. If another health condition makes CPAP use intolerable, ineffective, or aggravates your symptoms, you may still qualify for a 50% VA rating or even reach 100% in severe cases.
In 2022, VA proposed revising DC 6847 to consider comorbidities such as Parkinson’s, facial disfigurement, missing limbs, skull fractures, or contact dermatitis that prevent or impede treatment use. These conditions may help qualify veterans for higher ratings of 50% or 100%, since they directly interfere with safe, effective treatment of service-connected sleep apnea.
See: 87 Fed. Reg. 8474 (Feb. 15, 2022)
If these comorbidities prevent CPAP use or worsen sleep apnea, they directly support a higher VA disability rating for sleep apnea.
How to Get a Higher VA Rating for Sleep Apnea
Whether you’re filing a new claim or trying to increase your rating, use these strategic tips:
1. File an Intent to File (ITF) immediately with the assistance of a legal professional if needed.
Submitting VA Form 21-0966 now secures your effective date and locks you into the current, more favorable sleep apnea rating system. This step can preserve eligibility for the 50% CPAP rating and ensure you don’t lose out on back pay or compensation once the stricter rules take effect.
2. Get a VA-Recognized Sleep Study Diagnosis
The VA will not rate sleep apnea without a valid polysomnography (sleep study), whether in-lab or at-home, since it confirms breathing disruptions, oxygen levels, and brain activity. If your study is over a year old, get an updated one to show worsening symptoms, incomplete relief, or treatment effectiveness under the upcoming 2025 criteria.
3. Obtain a CPAP Prescription or Medical Recommendation
To qualify for the current 50% rating, you must have a prescription or recommendation for a CPAP or alternative device from a VA or private doctor. Compliance isn’t required under existing rules, but the prescription itself is what secures this rating.
4. Secure a Nexus Letter Linking Sleep Apnea to Service when applicable
A nexus letter from a qualified medical provider aims to connect your sleep apnea to service-related conditions like PTSD, GERD, or sinusitis. This independent medical opinion is often the deciding factor in getting approval for both direct and secondary service connection claims.
5. Document CPAP Ineffectiveness or Inability to Use
Since the VA is shifting to treatment-outcome-based ratings, you need proof that your CPAP is either ineffective or is intolerable due to limitations such as claustrophobia, skin irritation, or comorbidities. Supporting evidence such as updated sleep studies, treatment notes, and personal statements will be crucial for maintaining or increasing your VA rating under the proposed system.
6. Be Thorough but Honest in Your C&P Exam
During your Compensation & Pension (C&P) exam for sleep apnea, describe all symptoms truthfully, including daytime fatigue, cognitive issues, or CPAP side effects. Don’t minimize or exaggerate. When completing a Sleep Apnea Disability Benefits Questionnaire (DBQ) at your C&P exam, provide accurate details about your condition and its functional impact, as the examiner’s notes often carry more weight than your file.
7. Consider Secondary Claims for Increased Compensation
Sleep apnea frequently contributes to secondary conditions like hypertension, atrial fibrillation, GERD, or depression. Filing for these conditions with supporting medical evidence can increase your overall combined VA rating and monthly compensation, while also corroborating the service connection for your primary sleep apnea claim.
Disclaimer: This article is for educational purposes and is not legal or medical advice. Veterans should consult a qualified clinician and/or accredited representative for guidance on their case.
Conclusion
While myths often cloud the VA disability claims process, the truth is that documented medical necessity and accurate records hold the most importance in securing benefits linked with a CPAP rating. Compliance may not define your rating today, but it does help manage your apneic episodes and boost future claims. If you’re struggling with CPAP, filing before the rating change effective date can protect your benefits under the existing rules. Ultimately, clear medical evidence and honest communication with your providers remain the powerful tools for safeguarding your VA rating.
FAQs
What is acceptable CPAP compliance?
Acceptable compliance is using CPAP at least 4 hours per night on 70% of nights over a 30-day period, though this is for health purposes, not VA rating requirements.
What is the VA rating for CPAP?
Under current rules, a prescribed CPAP qualifies most veterans for a 50% disability rating for sleep apnea.
How to prove CPAP compliance?
You can show compliance through CPAP machine data, medical records, or follow-up visits, though it is not required for the VA to grant the 50% rating.
Is it a mandatory 50 percent if issued a CPAP by the VA?
Yes, if a CPAP is medically prescribed for sleep apnea, it generally results in a 50% rating under Diagnostic Code 6847.
What is the VA rating for CPAP machines?
A CPAP prescription for sleep apnea typically qualifies for a 50% VA disability rating.
How much is a 50% VA disability for sleep apnea?
As of 2025, a veteran rated 50% (without dependents) receives $1,102.04 per month in VA disability compensation.
View the official table for current amounts: VA disability compensation rates.
Is sleep apnea eligible for VA disability?
Yes, sleep apnea is a recognized condition eligible for VA disability benefits if diagnosed and linked to service.
Also read: Is Sleep Apnea Presumptive Under the PACT Act for VA Disability?
At Prestige Veteran Medical Consulting, a veteran-owned company, we specialize in Independent Medical Opinions (IMOs) known as Nexus letters.
Our purpose is to empower YOU, the veteran, to take charge of your medical evidence and provide you with valuable educational tools and research to guide you on your journey.
Understanding the unique challenges veterans face, our commitment lies in delivering exceptional service and support.
Leveraging an extensive network of licensed independent medical professionals, all well-versed in the medical professional aspects of the VA claims process, we review the necessary medical evidence to incorporate in our reports related to your VA Disability Claim.
Prestige Veteran Medical Consulting is not a law firm, accredited claims agent, or affiliated with the Veterans Administration or Veterans Services Organizations. However, we are happy to discuss your case with your accredited VA legal professional.