While many veterans are familiar with the term “sleep apnea,” fewer understand that it exists in different forms, most notably Obstructive Sleep Apnea (OSA) and Central Sleep Apnea (CSA). There’s also a hybrid form, known as Complex Sleep Apnea Syndrome, that combines features of both.
Understanding the difference between central and obstructive sleep apnea is crucial not only for treatment but also for determining how the U.S. Department of Veterans Affairs (VA) evaluates and rates disability claims.
Table of Contents
Types of Sleep Apnea: A Clinical Overview
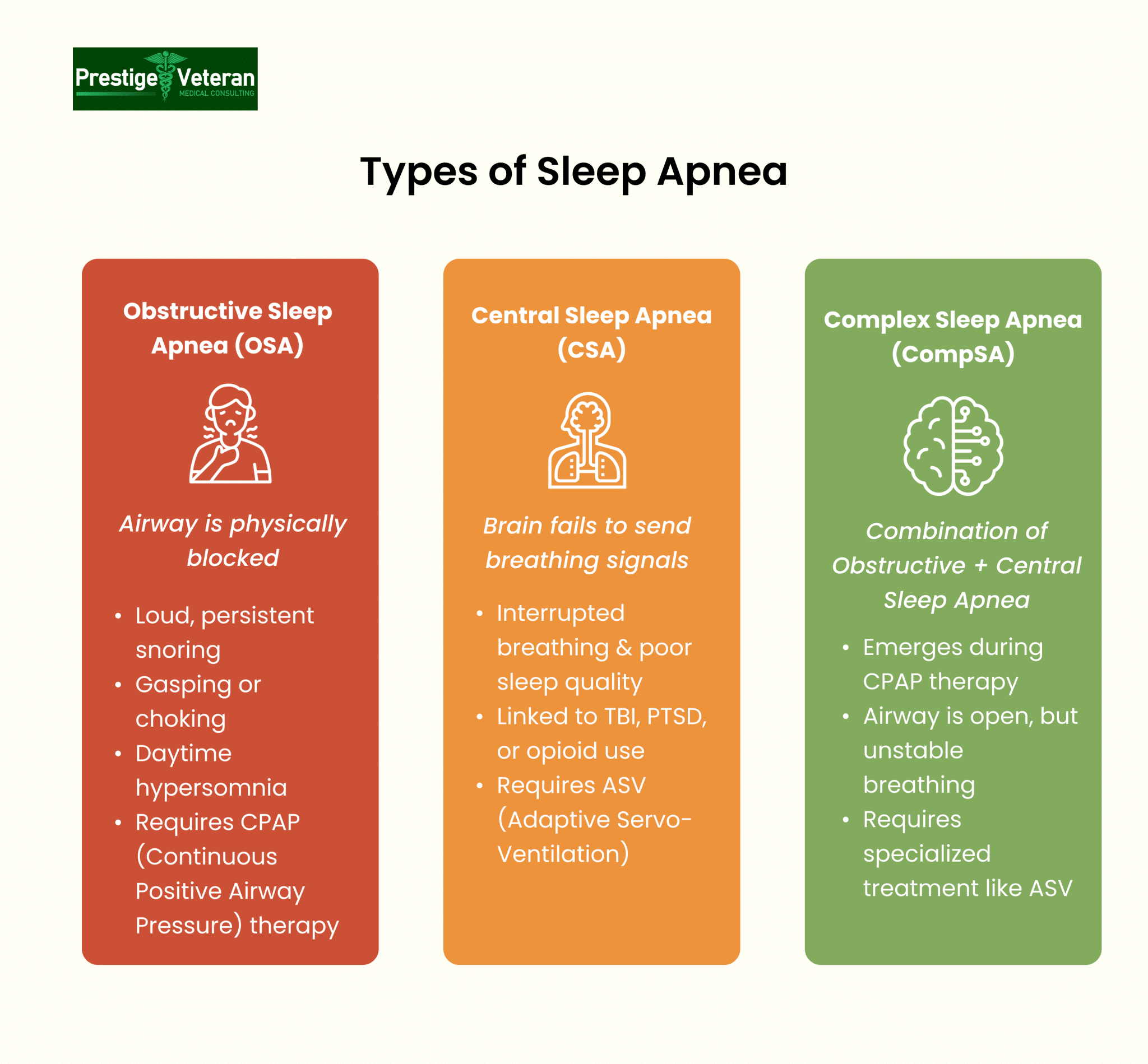
Sleep apnea is a chronic respiratory disorder that can significantly affect a veteran’s health, daily functioning, and overall quality of life. The U.S. Department of Veterans Affairs (VA) recognizes all types of sleep apnea as a compensable condition when linked to military service. There are three primary forms:
- Obstructive Sleep Apnea (OSA) – Caused by physical blockages in the upper airway.
- Central Sleep Apnea (CSA) – Caused by the brain failing to signal the body to breathe.
- Complex Sleep Apnea Syndrome (CompSA) – A mix of OSA and CSA, often emerging during CPAP therapy.
Each type may qualify for VA disability benefits under Diagnostic Code 6847. Understanding the differences between central and obstructive sleep apnea is essential for accurate diagnosis, proper treatment, and building a strong claim to maximize your VA rating.
What Is Obstructive Sleep Apnea?
Obstructive Sleep Apnea (OSA) is the most common form of sleep-disordered breathing, affecting a significant number of U.S. veterans. OSA occurs when the soft tissues in the back of the throat relax excessively during sleep, narrowing or completely blocking the upper airway. This obstruction prevents air from entering the lungs despite continued respiratory effort. As a result, oxygen levels drop, and the brain briefly awakens the body to resume breathing. These apneic episodes can happen dozens or even hundreds of times per night.
Obstructive Sleep Apnea Symptoms
- Loud, chronic snoring
- Gasping or choking during sleep
- Witnessed apneas (pauses in breathing)
- Excessive daytime sleepiness (hypersomnia)
- Poor concentration or memory issues
- Morning headaches
- Irritability or mood swings
ICD Code for Obstructive Sleep Apnea
The diagnostic code G47.33 corresponds to obstructive sleep apnea in the ICD-10 classification system and is routinely used in VA disability claims and sleep study documentation.
Why Is OSA Prevalent in Veterans?
Veterans are disproportionately affected by OSA due to a range of contributing factors:
- Weight gain after service due to injury, PTSD, or reduced activity.
- Toxic exposures (e.g., burn pits) causing airway inflammation. Powell et al. (2020) found that among 100 previously deployed service members, OSA prevalence was high in both burn-pit–exposed (69%) and unexposed (71%) groups.
- PTSD and anxiety, which disturb sleep architecture. A study of 195 Iraq and Afghanistan veterans found that 69.2% were at high risk for obstructive sleep apnea, and the risk increased as PTSD symptoms became more severe.
- Increased alcohol use and sedative medications, both of which relax airway muscles.
- Sleep disruptions during service (night shifts, field duty) leading to maladaptive sleep patterns.
Treatment for obstructive sleep apnea often involves the use of Continuous Positive Airway Pressure (CPAP) therapy, oral appliances, weight management, or surgery to keep the airway open during sleep.
What Is Central Sleep Apnea?
Central Sleep Apnea (CSA) is a less common but equally serious sleep disorder where breathing repeatedly stops and starts because the brain fails to send proper signals to the muscles that control breathing. Unlike obstructive sleep apnea, it’s not caused by a physical blockage of airflow but by instability in the brain’s respiratory control center. This interruption in breathing leads to low oxygen levels, fragmented sleep, and increased cardiovascular stress.
Central Sleep Apnea Symptoms
- Pauses in breathing during sleep (apneas)
- Poor sleep quality or insomnia
- Excessive daytime sleepiness (despite “full” nights of sleep)
- Morning headaches
- Mood swings or depression
- Trouble focusing
- Snoring (less prominent or absent compared to OSA)
Risk Factors in Veterans
Among Veterans, CSA is gaining attention due to its strong links with service-connected conditions such as traumatic brain injury (TBI), post-traumatic stress disorder (PTSD), and heart failure. Central sleep apnea can be particularly prevalent in veterans using opioid medications for chronic pain or suffering from neurological damage.
Treatment for central sleep apnea focuses on stabilizing breathing through adaptive servo-ventilation (ASV), oxygen therapy, or managing underlying issues. The VA is starting to offer an implantable diaphragm stimulator to treat moderate to severe CSA in veterans, aiming to reduce dependence on PAP machines.
Forms of Central Sleep Apnea
Central sleep apnea has several subtypes, each with unique causes:
- Cheyne-Stokes Respiration – Seen in heart failure or post-stroke patients, characterized by alternating periods of deep and shallow breathing. A review by Yumino & Bradley (2008) found that Cheyne-Stokes respiration with central sleep apnea in heart failure patients arises from unstable ventilatory control and leads to sympathetic activation, hypoxia, and increased mortality.
- Medication-Induced Apnea – Opioids, sedatives, or benzodiazepines can suppress the brain’s respiratory drive. In a 2015 review by Correa et al., 8 studies involving 560 chronic opioid users revealed that 24% had central sleep apnea, with higher opioid doses, low BMI, and sedative use increasing risk.
- High-Altitude CSA – Triggered by low oxygen levels at elevation.
- Treatment-Emergent CSA – Appears during CPAP (Continuous Positive Airway Pressure) treatment for obstructive sleep apnea. Mador (2017) in the Journal of Thoracic Disease reported that central sleep apnea emerging during CPAP therapy occurs in approximately 5% to 20.3% of patients, with an overall average prevalence of about 8.4%.
- Idiopathic (Primary) CSA – No known underlying cause, but is often linked to neurological irregularities.
Different Root Cause Compared to OSA
While Obstructive Sleep Apnea (OSA) results from a mechanical issue involving tissue obstruction of the airway, Central Sleep Apnea (CSA) arises from a neurological failure in the brain’s respiratory control center. During CSA, the brain intermittently “forgets” to signal the muscles to breathe, while in OSA, the body is trying to breathe but is physically blocked.
Understanding this root difference is essential for accurate diagnosis, determining VA disability ratings and therapies, and establishing secondary service connections.
Central vs. Obstructive Apnea: Top Differences
| Feature | Obstructive Sleep Apnea (OSA) | Central Sleep Apnea (CSA) |
| Cause | Physical blockage of the airway | Failure of the brain to signal breathing |
| Snoring | Very common and loud | Less frequent, quieter |
| Awakening episodes | Choking, gasping, snorting | Subtle, often unnoticed |
| Underlying risk factors | Obesity, toxic exposure, PTSD, sleep disturbances | Heart failure, stroke, brainstem damage |
| Treatment | CPAP, oral devices, surgery | ASV, BiPAP, treating the underlying condition |
| ICD-10 Code | G47.33 | G47.37 |
Hypopnea vs Obstructive Apnea in VA Disability Claims
While an apnea represents a complete pause in breathing for at least 10 seconds, a hypopnea is a partial reduction in airflow that still leads to oxygen desaturation and sleep disruption. Both are significant indicators of sleep-disordered breathing.
- Obstructive Hypopneas: Caused by partial airway collapse or narrowing during sleep.
- Central Hypopneas: Result from reduced brain signals controlling the breathing muscles, without physical blockage.
Understanding these events is vital during a polysomnography (sleep study), as both contribute to the Apnea-Hypopnea Index (AHI), the key metric used by the VA rating system to evaluate sleep apnea severity and assign disability ratings.
Complex Sleep Apnea (CompSA): The Overlap
Complex Sleep Apnea Syndrome (CompSA), also known as treatment-emergent central sleep apnea, occurs when features of both obstructive sleep apnea (OSA) and central sleep apnea (CSA) are present. It typically develops in patients initially diagnosed with OSA and begin continuous positive airway pressure (CPAP) therapy, only to develop central apneas during treatment.
This happens because the sudden change in breathing pressure and oxygen balance can disrupt the brain’s respiratory control system, leading to unstable breathing patterns. As a result, even though airway blockages are resolved, breathing irregularities persist.
Since this condition reflects a unique interplay between the two kinds of sleep apnea, central and obstructive, specialized therapies such as adaptive servo-ventilation (ASV) are often needed to restore stable breathing and improve sleep quality.
VA Disability Ratings: Does the Type of Apnea Matter?
Both central and obstructive sleep apnea are eligible for VA disability compensation under Diagnostic Code 6847. The VA does not rate these conditions differently based on their cause but rather on the severity of symptoms and required treatments.
VA Sleep Apnea Ratings (38 CFR § 4.97, DC 6847)
- 0% – Asymptomatic with documented sleep-disordered breathing.
- 30% – Persistent daytime hypersomnolence.
- 50% – Requires use of a breathing assistance device (e.g., CPAP or BiPAP).
- 100% – Chronic respiratory failure with CO₂ retention, cor pulmonale, or tracheostomy.
Important Note:
At present, DC 6847 assigns a 50% rating when the use of a breathing-assistance device is required. However, the VA has proposed changes to this rule, specifically, whether CPAP use alone should continue to justify a 50% evaluation when the device fully controls symptoms.
For details, see the Federal Register proposed rule update published on February 15, 2022 (87 FR 8474), with a supplemental notice issued on September 12, 2024 (89 FR 74162). Veterans with pending claims are encouraged to submit now to preserve current rating guidelines.
For an in-depth breakdown of how these proposed updates could impact future ratings, visit our guide on VA sleep apnea rating changes.
Evidence Needed for Obstructive & Central Sleep Apnea Claims
When veterans file VA disability claims for obstructive central, or complex sleep apnea, the right evidence can result in a successful claim. The VA may evaluate them differently, particularly when it comes to causation and service connection.
According to M21-1, Part V, Subpart ii, Chapter 1, Section A, establishing service connection for sleep apnea requires three key evidence:
- A confirmed medical diagnosis
- Documentation of an in-service event, injury, or illness
- A well-supported medical nexus linking the condition to military service
Together, these elements lay the foundation of a VA claim, which can be supported by the following documented evidence.
Sleep Study Results (Polysomnography)
The VA rarely accepts a sleep apnea diagnosis without a polysomnography. This overnight test, often performed in a clinical lab, confirms the diagnosis and specifies whether the apnea is obstructive, central, or complex by tracking breathing patterns, oxygen levels, and brain activity.
For instance, an Army veteran’s in-lab test may reveal that their apneic episodes stem from neurological causes (CSA) rather than airway collapse (OSA), a key detail for accurate rating and medical linkage.
CPAP Prescription as Key Evidence
A Continuous Positive Airway Pressure (CPAP) prescription demonstrates that the condition requires ongoing, device-assisted treatment, a key factor in higher VA ratings (commonly 50%).
Under 38 CFR §4.97, Diagnostic Code 6847, a CPAP or BiPAP prescription often supports entitlement to a 50% VA disability rating.
To strengthen a CPAP rating claim, veterans can include:
- Copies of their initial and updated prescriptions
- Equipment setup documentation
- Compliance or usage reports from the machine
- Follow-up notes from their VA or private providers verifying ongoing therapy
These documents establish both the chronic nature of the condition and the necessity of ongoing respiratory support, reinforcing eligibility for higher compensation.
Treatment Records
Veterans should submit comprehensive treatment records that document the severity and continuity of their sleep apnea. These records help show when the condition was first diagnosed, its response to therapy, and any adjustments made to treatment, such as changing from CPAP to BiPAP for central apneas. It also helps the VA determine whether the apnea is obstructive, central, or complex, and whether it worsened due to service-related factors or secondary conditions.
Key elements to include:
- Initial diagnosis date and sleep study results.
- Notes showing treatment-emergent central sleep apnea developed while using CPAP.
- Records of persistent symptoms like daytime hypersomnolence, insomnia, or morning headaches.
- Documentation of associated conditions, such as heart failure or brain injury, which can aggravate CSA.
Accurate records demonstrate ongoing challenges, validate treatment compliance, and support the need for medical care or disability benefits related to service-connected sleep apnea.
Medical Nexus Letters (Especially for CSA and Complex Cases)
A nexus letter linking sleep apnea to military service or a service-connected condition (such as PTSD, traumatic brain injury, hypertension, or cardiac disease) may prove to be crucial evidence. Central and Complex Sleep Apnea VA claims, in particular, often require expert analysis to explain neurologic or cardiovascular causes that trace back to service.
The nexus letter or an independent medical opinion should:
- Be written by a qualified medical provider.
- Reference the veteran’s military history and medical records.
- Provide a clear medical opinion using VA-accepted terminology that it is “at least as likely as not (50% probability or greater)” that the condition is connected to service.
- A detailed pathophysiologic explanation linking service-related factors to the current diagnosis
- Provide rationale supported by medical literature or the VA’s rating criteria (38 CFR).
For example, a veteran with service-connected PTSD and newly diagnosed central sleep apnea may need a physician to explain how chronic hyperarousal, anxiety-related breathing irregularities, or side effects of PTSD medications contributed to the development of CSA. Without this letter, the VA may argue that CSA is the result of post-service weight gain or non-service-related factors.
Lay Evidence: First-Hand Observations
Statements from spouses, roommates, or fellow service members are powerful supporting evidence in a VA claim. They can confirm early symptoms like loud snoring, gasping, or pauses in breathing, especially if no in-service diagnosis was made. This type of lay evidence submitted on VA Form 21-4138 (Statement in Support of Claim) can help establish the onset of symptoms before a formal diagnosis and support service connection.
A fellow service member may state, “When we were stationed together, I often heard him snoring loudly and noticed he would stop breathing for several seconds before gasping or waking up suddenly.”
How to File a VA Disability Claim for Sleep Apnea
For veterans managing sleep apnea, filing a VA disability claim becomes much easier when you understand what documentation is needed and how to submit it correctly.
Step 1: Gather Medical Evidence
Obtain a confirmed sleep apnea diagnosis through a VA-approved sleep study that specifies whether it’s OSA, CSA, or CompSA. Include CPAP/BiPAP prescriptions, treatment records, and compliance data.
Step 2: Complete VA Form 21-526EZ
File your claim using VA Form 21-526EZ (“Application for Disability Compensation and Related Compensation Benefits”). Attach service-related documentation linking your condition to duty, nexus letters from a qualified provider, and lay evidence.
Step 3: Submit Your Claim
Finally, submit your disability benefits claim securely online through VA.gov, by mail, or in person at your regional VA office. Keep copies of all submissions.
Step 4: Attend C&P Examination
If scheduled, attend the Compensation & Pension (C&P) exam, where a VA clinician will review your medical history, sleep study, and symptoms to confirm severity and service connection.
Step 5: Track Your Claim & Respond Promptly
Monitor your claim status online. Provide any additional records requested by the VA to avoid delays and ensure a fair, timely decision on your disability rating.
By following the official process outlined by the U.S. Department of Veterans Affairs, you can ensure your claim is complete and well-supported.
Why Sleep Apnea VA Claims Get Denied
If your sleep apnea claim is denied, you have the option to file a Supplemental Claim, request a Higher-Level Review, or submit a Board Appeal. Understanding these common reasons for denial can help you build stronger cases:
- No nexus opinion connecting the condition to military service or an existing service-connected disability.
- VA attributing apnea to post-service weight gain rather than service-related causes, especially common with obstructive sleep apnea (OSA).
- Lack of a documented sleep study or inconsistent medical evidence of diagnosis and treatment.
Veterans filing claims involving obstructive or central sleep apnea must understand that CSA is frequently presumed to be caused by non-service-connected conditions unless specifically argued and supported.
VA’s General Respiratory Formula and Future Changes
Right now, all forms of sleep apnea: obstructive, central, and complex, are rated under Diagnostic Code 6847. The rating hinges on symptoms and prescribed treatments, not the exact type of apnea. For example, if a veteran requires a CPAP, the rating is typically 50 percent, regardless of whether the condition is obstructive or central in origin.
However, the VA has been reviewing the respiratory section of the Schedule for Rating Disabilities, with the possibility of shifting to a general respiratory formula. If this change takes place, it could significantly alter how sleep apnea claims are evaluated.
Under a general respiratory formula, the VA would focus less on whether a CPAP or BiPAP is prescribed and more on objective respiratory impairment. Instead of relying on treatment devices as rating triggers, the system could use measurable factors such as:
- Blood gas levels (PaCO₂ retention or oxygen saturation).
- Pulmonary function tests (FEV-1, FVC, or DLCO scores).
- Evidence of cor pulmonale or chronic respiratory failure.
Impact on Veterans’ Disability Claims
This would bring sleep apnea ratings more in line with other respiratory conditions like asthma or COPD, which are already assessed by test results and functional impact.
For veterans with central sleep apnea (CSA), this shift could cut both ways. On one hand, many CSA cases are not treated effectively with CPAP, so veterans may currently struggle to reach the 50 percent level. A general respiratory formula could open the door to ratings based on severity rather than device usage. On the other hand, veterans with mild obstructive apnea but a CPAP prescription might find it harder to qualify for a 50% VA rating if future rules require evidence of measurable respiratory dysfunction.
In short, the VA has not yet adopted these changes, but veterans should be aware: the rating schedule is evolving, and future updates may place greater weight on test results and functional limitations rather than simply the type of device prescribed.
Conclusion
Ultimately, the VA does not rate central and obstructive sleep apnea differently by type but rather by severity, treatment needs, and functional impact. However, veterans must still clearly establish the origin, service connection, and ongoing medical necessity to secure fair compensation.
Whether your diagnosis is obstructive or central, focus on obtaining thorough documentation, consistent treatment, and a strong medical nexus letter. As rating standards evolve, informed veterans who stay proactive and detailed in their sleep apnea VA claims will be best positioned for long-term benefits.
FAQs
What’s the difference between central and obstructive sleep apnea?
Obstructive sleep apnea is caused by a physical airway blockage, while central sleep apnea results from the brain failing to signal the body to breathe.
What is the VA rating for complex sleep apnea?
Complex sleep apnea is rated under Diagnostic Code 6847 based on symptom severity and treatment needs, just like other forms of sleep apnea.
Can I secure a 50% VA rating if issued a CPAP by the VA?
Yes, a prescribed CPAP typically supports a 50% VA disability rating under current guidelines.
Does the VA rate obstructive, central, and complex sleep apnea differently?
No, the VA rates all types of sleep apnea under the same code (6847) based on severity and treatment, not the specific type.
Does central sleep apnea qualify for disability?
Yes, central sleep apnea qualifies for VA disability compensation if properly diagnosed and connected to military service.
How to get VA disability benefits for obstructive sleep apnea?
You need a confirmed sleep study diagnosis, a CPAP prescription or treatment record, a medical nexus, and lay evidence linking the condition to military service.
What evidence does the VA need for sleep apnea?
The VA requires a sleep study, treatment documentation (like CPAP use), medical nexus letters, and supporting lay statements to substantiate a claim.
Also read: How to Get a Nexus Letter for Sleep Apnea? (Sample Template Included)
At Prestige Veteran Medical Consulting, a veteran-owned company, we specialize in Independent Medical Opinions (IMOs) known as Nexus letters.
Our purpose is to empower YOU, the veteran, to take charge of your medical evidence and provide you with valuable educational tools and research to guide you on your journey.
Understanding the unique challenges veterans face, our commitment lies in delivering exceptional service and support.
Leveraging an extensive network of licensed independent medical professionals, all well-versed in the medical professional aspects of the VA claims process, we review the necessary medical evidence to incorporate in our reports related to your VA Disability Claim.
Prestige Veteran Medical Consulting is not a law firm, accredited claims agent, or affiliated with the Veterans Administration or Veterans Services Organizations. However, we are happy to discuss your case with your accredited VA legal professional.













