Last Updated on 28 August, 2025
Post-traumatic stress disorder (PTSD) is a serious mental health condition that many veterans may face as a result of their service. When filing a claim for PTSD or seeking an increase in compensation for an existing service-connected PTSD, veterans often undergo a Compensation and Pension (C&P) exam. Let’s explore what to expect during a PTSD C&P exam, including the process and the Disability Benefit Questionnaire (DBQ).

Table of Contents
What Is a C&P Exam for PTSD?
A Compensation and Pension (C&P) exam for PTSD is a medical evaluation ordered by the U.S. Department of Veterans Affairs (VA) once a veteran files a disability claim for post-traumatic stress disorder. Even if you already carry a diagnosis from a VA psychiatrist, private PTSD doctor, or trauma therapist, the VA requires this independent evaluation to confirm the diagnosis, establish a service connection, and assess severity under the VA’s Schedule for Rating Disabilities (38 CFR §4.130).
Unlike therapy sessions, this exam is not designed to provide treatment. Instead, the examiner, usually a VA psychologist, psychiatrist, or contracted provider, documents findings on your mental health symptoms, which becomes a cornerstone of your PTSD claim. In some instances, other medical professionals, like psychiatric nurse practitioners under supervision, may also perform these exams.
Because the VA places significant weight on the examiner’s opinion, the outcome of your VA PTSD exam can dramatically affect your rating. For example, if the examiner concludes your symptoms are “mild” when they are actually moderate, your rating could be 10% instead of 30% or higher. In short, the PTSD C&P exam often determines whether a veteran receives the full benefits they’ve earned.
Who Needs a PTSD C&P Exam?
Most veterans who file a VA PTSD claim will be scheduled for a C&P exam. The VA uses this exam to confirm the diagnosis, validate the stressor, and determine how severely the condition impacts daily life.
You will almost certainly need a C&P exam for PTSD if:
- You’re filing an initial PTSD claim – Veterans filing an initial PTSD claim must attend a VA PTSD examination to confirm the diagnosis and validate the in-service stressor (e.g., combat trauma, IED blast, or military sexual trauma).
- You’re requesting a rating increase – If your symptoms have worsened since your last decision, you may undergo a review C&P exam for PTSD increase, with the examiner completing a new DBQ to reassess severity.
- The VA requires a reexamination – Some veterans are called for periodic exams to confirm their condition has not improved significantly.
- You’re filing an MST-related claim – Veterans filing PTSD claims for military sexual trauma (MST) often face exams focused on “markers” in service records, such as behavioral changes or disciplinary actions.
- You’re filing a secondary or complex claim – Veterans with PTSD often develop conditions like depression, anxiety, substance use, or sleep apnea. When these are linked to PTSD, the VA may order another C&P exam to evaluate both conditions together.
Example: A veteran who originally received a 30% rating for nightmares and hypervigilance might later request a reevaluation if panic attacks, social isolation, and work impairment worsen. The VA may schedule a 2nd C&P exam for PTSD to determine if the VA rating increase is justified.
If you receive a notice for a PTSD C&P exam, attendance is mandatory. Missing it without any valid reason almost always results in denial.
The 3 Types of PTSD C&P Exams for Veterans
If you are a Veteran pursuing VA disability benefits for PTSD, understanding the types of Compensation & Pension (C&P) exams is essential. Each exam serves a specific purpose in your disability claim journey and is critical to securing accurate ratings aligned with VA criteria.
Types of PTSD C&P Exams:
- Initial PTSD Evaluation – For veterans filing their first PTSD claim. Establishes diagnosis, documents symptoms, and connects them to your military service, whether combat or non-combat.
- PTSD Re-Evaluation Exam – Also known as Review Exam, this evaluation applies to already rated Veterans seeking a higher VA rating due to worsening of symptoms.
- Specialized Trauma-Focused Exam – Focuses on non-combat PTSD, such as Military Sexual Trauma (MST), harassment, or assault.
These exams may be conducted by VA or non-VA mental health professionals, but all follow forensic protocols required by the Veterans Benefits Administration. Veterans must be prepared and informed to ensure their condition is properly documented.
PTSD DBQ and DSM-5 Criteria: A Comprehensive Evaluation
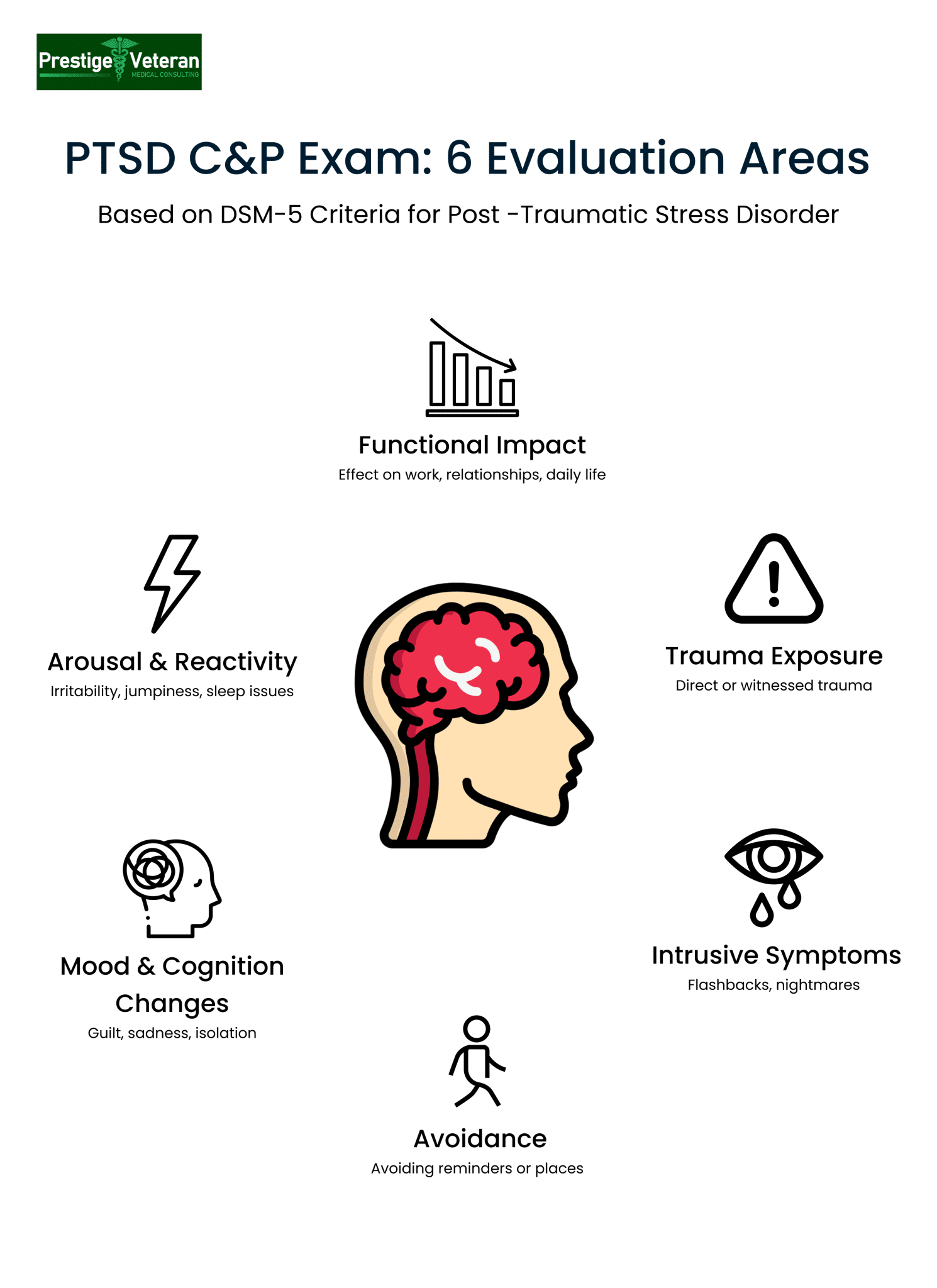
The PTSD Disability Benefits Questionnaire (DBQ) is the standardized form used in every VA PTSD C&P exam. The questionnaire ensures each aspect of a veteran’s condition is evaluated according to 38 CFR §4.130, Diagnostic Code 9411.
The DBQ is designed to guide the examiner through all factors the VA considers when assigning or adjusting a disability rating. During the exam, the examiner determines whether a veteran meets the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5) criteria for Post-Traumatic Stress Disorder. This has replaced the GAF (Global Assessment of Functioning) scale used to be a standard part of VA mental health evaluations.
DSM-5 Criteria for Verifying PTSD
Criteria A: Exposure to Traumatic Events
The DBQ’s diagnostic criteria section begins by addressing whether the veteran has ever been diagnosed with PTSD. It explores the nature of traumatic events like combat, MST, accident, etc., covering direct experiences, witnessing or learning about traumatic events happening to close family members or friends.
Criteria B: Intrusion Symptoms
This section delves into intrusion symptoms associated with the traumatic event, such as distressing memories, dreams, and dissociative reactions (flashbacks).
Criteria C: Persistent Avoidance of Stimuli
Here, the questions are focused on persistent avoidance of distressing memories, thoughts, or external reminders related to the traumatic event.
Criteria D: Negative Alterations in Cognitions and Mood
The DBQ evaluates negative alterations in cognition and mood associated with the traumatic event, such as distorted beliefs, persistent negative emotions like guilt or hopelessness, diminished interest in significant activities, and isolation.
Criterion E: Marked Alterations in Arousal and Reactivity
The examiner records clinical findings, including observable behaviors such as irritable or reckless behavior, hypervigilance, exaggerated startle responses, concentration problems, and sleep disturbances.
Criterion F: Duration
Symptoms satisfying Criteria B, C, D, and E must persist for more than one month. If less, the veteran does not meet full PTSD criteria.
Criterion G: Functional Impact
PTSD symptoms must interfere in a significant way with daily life, such as distress or impairment in social, occupational, or other important areas of functioning. If they do not create noticeable impact, full diagnostic criteria for PTSD are not satisfied.
Criterion H: Differential Exclusion
Examiners ask questions about whether the disturbance is not solely due to the psychological effects of substances or medications.
Additional Considerations
Apart from the detailed questioning, the examiner reviews evidence, including recent history, relevant social and family history, occupational and educational history, and legal and behavioral history. A DBQ for Post-Traumatic Stress Disorder will also note down if the veteran also has comorbid conditions such as depression, anxiety, or TBI.
Example: A veteran reporting “3–4 nightmares weekly, avoids grocery stores due to panic, isolates from spouse, and startles easily at loud noises” likely meets full DSM-5 criteria.
Impact on VA Disability Claim
The DBQ is critical because it directly informs your VA PTSD rating. Based on the information recorded in the form, the examiner gives a nexus opinion on whether the PTSD is “at least as likely as not” related to an in-service stressor.
If symptoms are documented inaccurately or omitted during the examination, your compensation may not reflect the actual life impact. Hence, reviewing the DBQ form before your exam helps you understand what evidence matters most to prove service connection.
Download the official PTSD Disability Benefits Questionnaire (DBQ) directly from the VA website.
How to Prepare for the Exam
Upon initiating a claim for PTSD, veterans typically receive a packet containing essential details about their C&P exam. This information includes the location, the examiner’s details, and, in some cases, the examiner’s experience in conducting such evaluations.
Here’s a simple day-by-day preparation approach veterans can follow leading up to PTSD C&P exam day:
1 Week Before the Exam:
- Gather all medical evidence: VA and private treatment notes, therapy records, prescriptions, and any nexus letters from a PTSD doctor.
- Review your submitted VA Form 21-0781 (stressor statement) to refresh what you’ve already shared.
5 Days Before the Exam:
- Begin a symptom diary. Write down examples of nightmares, panic attacks, anger outbursts, or times you avoided social situations. Example: “Skipped family gathering due to anxiety—heart pounding, sweating, couldn’t speak.”
- Ask your spouse, friend, or coworker for a short buddy statement describing how PTSD affects your daily functioning.
3 Days Before the Exam:
- Review the PTSD DBQ so you understand the criteria the examiner will cover.
- Organize notes on your “worst days” to avoid downplaying mental health symptoms.
1 Day Before the Exam:
- Avoid alcohol or sedatives (unless prescribed) that might blunt symptoms.
- Pack treatment records, a written symptom log, and a list of medications.
Day of the Exam:
- Arrive early, as examiners sometimes note punctuality.
- Stay calm but honest; don’t exaggerate, but don’t minimize. If nightmares prevent restful sleep, say so.
- Remember: Examiners observe you from the waiting room onward. Grooming, affect, and body language may often appear in reports.
This detailed preparation ensures you present an honest picture of your PTSD during the exam.
What Happens During the Exam (Start to Finish)
A PTSD C&P exam usually lasts 60–90 minutes, though times vary by examiner. Understanding what actually happens during the appointment can reduce anxiety and help you stay focused. Here’s the typical process:
1. Check-In & File Review
The examiner greets you and confirms your identity. They may have already reviewed your claims file (C-file), including service treatment records, stressor statements, and prior medical notes. Veterans should never assume that the VA examiners have studied every page, and hence be ready to highlight key points.
2. Medical & Military Trauma History
You’ll be asked about your service background, deployment details, and the traumatic events you experienced in active duty. Be as direct as you can. For example, “During deployment in Iraq, our convoy hit an IED. I saw fellow soldiers killed, and I still replay those images every night.”
3. Symptom Exploration
Expect detailed questions about your PTSD symptoms linked to military service:
- Nightmares, flashbacks, or intrusive thoughts
- Avoidance behaviors (e.g., avoiding crowds, highways, or certain uniforms)
- Mood changes such as guilt, shame, or anger
- Hypervigilance and exaggerated startle response
- Substance use as a coping mechanism
4. Functional Impact
The examiner assesses how current PTSD interferes with work, school, relationships, and self-care. Example questions:
- “How often do you miss work due to anxiety?”
- “How has PTSD affected your marriage or friendships?”
- How frequent do panic attacks occur, and what triggers them?
5. Psychological Testing
Many PTSD C&P exams include written or verbal tests, such as the PTSD Checklist for DSM-5 (PCL-5), the MMPI-2, or the M-FAST (used to detect malingering). These tests can become a part of your record; hence, it is important to answer honestly. While controversial, results of psychological testing may influence your VA disability rating.
6. Mental Status Exam
During the mental status exam, the VA examiner observes appearance, speech, thought process, mood, memory, and insight. For example, they may note “the veteran appeared disheveled, with restricted affect and anxious mood.”
7. Completion of DBQ
Finally, the examiner records findings on the Disability Benefits Questionnaire for PTSD. This DBQ form documents whether you meet DSM-5 diagnostic criteria for PTSD, your symptom frequency, ability to manage finances, and, most importantly, assesses your level of occupational and social impairment. It is this last section of the C&P exam that greatly influences your VA rating.
End of Exam:
You will not receive a decision on the spot. The examiner submits their report to the VA, where a rater determines your percentage.
After the Exam
Once your PTSD C&P exam is conducted, the examiner submits the DBQ and reports to the VA. Note that you will not receive exam results immediately.
How Long Does It Take to Get Results?
You won’t receive results the day of your exam. The examiner submits the Disability Benefits Questionnaire (DBQ) and reports directly to the VA. From there, a rater reviews your entire file before making a decision. On average, veterans wait 120–150 days to receive a decision on their PTSD C&P exam. Your outcome will arrive by mail in a decision packet and may also appear sooner on VA.gov under your claims status.
What Are the Possible Outcomes?
Once the VA reviews your C&P exam, three results are possible:
- Grant of service connection with a percentage rating – If PTSD is confirmed and linked to service, you’ll receive a rating from 0% to 100%.
- Denial – If the examiner determines you don’t meet PTSD criteria, or the VA cannot connect it to service.
- Deferred decision – If more medical evidence is needed before a final ruling.
What Should You Do After Receiving the Decision?
When your decision letter arrives, request a copy of your C&P exam report from the VA. Compare the examiner’s notes with your lived experience and medical records.
If your rating is too low or denied, you can file a supplemental claim, request a Higher-Level Review, or appeal to the Board of Veterans’ Appeals.
Tip: After the exam, write down your impressions. Note whether the examiner listened, the length of the interview, and any inaccuracies. This record can support a challenge later.
Bad C&P Exam? Here’s How to Challenge It
Not every examination is fair or accurate. If you believe your VA PTSD C&P exam was rushed, dismissive, or incorrect, follow these steps:
- Step 1: Request a copy of your VA PTSD C&P exam report to review for inaccuracies, missing details, or contradictions with your treatment records.
- Step 2: Submit a written rebuttal highlighting errors, such as improper use of DSM-5 criteria or ignoring supporting statements from family and friends.
- Step 3: Obtain an Independent Medical Examination (IME) or a private DBQ for PTSD completed by a qualified psychiatrist, psychologist, or PTSD specialist.
- Step 4: File a Supplemental Claim by including new and relevant medical nexus or lay evidence to strengthen your case.
- Step 5: If needed, appeal the decision through a Higher-Level Review or escalate it to the Board of Veterans’ Appeals.
Example: One veteran was labeled “malingering” after scoring high on the M-FAST test. With an IMO from a private psychiatrist explaining chronic PTSD symptoms, the Board later granted a 70% rating.
While the C&P examiner’s opinion carries weight, it is not the final decision. Solid medical evidence and supporting documentation can successfully overturn a bad exam.
You can learn more about these VA decision review and appeal options on the official VA website.
What Does It Mean By a Veteran Is Malingering?
Malingering in a VA PTSD C&P exam refers to the intentional exaggeration or fabrication of symptoms for external gain, often financial compensation or avoidance of responsibility.
To assess malingering, VA examiners may administer psychological tests alongside the clinical interview. The M-FAST (Miller Forensic Assessment of Symptoms Test) is commonly used. It is a 25-item tool that evaluates seven domains, such as unusual symptom patterns, rare combinations, or inconsistencies between reported and observed behavior. A score of 6 or higher may flag possible malingering.
In some cases, examiners will follow up with other broader tests like the MMPI-2 (Minnesota Multiphasic Personality Inventory-2) or the PAI Personality Assessment Inventory, which include validity scales designed to detect exaggeration.
In a 2012 Army Medical Command Policy Memo (Policy Memo 12‑035, dated April 10, 2012), the Army stressed that “considerable evidence” indicates malingering is rare among veterans and cautioned that a diagnosis of malingering should only be made when “substantial and definitive evidence from collateral or objective sources” clearly demonstrates false or grossly exaggerated symptoms.
Malingering accusations can severely damage a claim. For example, if a veteran seeking a rating increase is mistakenly labeled as malingering, their DBQ for PTSD may be disregarded, and the claim denied.
If an examiner suggests malingering without strong evidence, the veteran can seek an Independent Medical Opinion (IMO) or nexus letter from a qualified doctor to challenge the claim.
PTSD VA Ratings & How the C&P Exam Impacts Your Percentage
When the VA assigns a disability rating for Post-Traumatic Stress Disorder (PTSD), it relies on the General Rating Formula for Mental Disorders found in 38 CFR §4.130. Ratings range from 0% to 100%, depending on how much your symptoms interfere with work and daily life.
Here is a table depicting the VA rating criteria for PTSD and the monthly compensation granted for each percentage in 2025:
|
Rating |
Description |
Monthly Compensation (No Dependents) |
|
0% |
PTSD is formally diagnosed, but symptoms are not severe enough to interfere with work or social functioning, nor do they require continuous medication. |
$0/month (No compensation) |
|
10% |
Mild or transient symptoms that decrease work efficiency and ability to perform occupational tasks only during periods of significant stress, or symptoms controlled by continuous medication. |
$175.51/month |
|
30% |
Occasional decrease in work efficiency with intermittent inability to perform occupational tasks. Common symptoms include depressed mood, anxiety, weekly or less frequent panic attacks, chronic sleep impairment, and mild memory loss. |
$537.42/month |
|
50% |
Reduced reliability and productivity due to symptoms such as flattened affect, panic attacks more than once a week, impaired judgment, memory issues, disturbances of motivation and mood, and difficulty maintaining relationships. |
$1,102.04/month |
|
70% |
Deficiencies in most areas (work, school, family, judgment, mood, or thinking). Symptoms may include suicidal ideation, near-continuous panic or depression, impaired impulse control, neglect of personal hygiene, or inability to handle stress. |
$1,759.19/month |
|
100% |
Total occupational and social impairment caused by severe symptoms such as gross impairment in thought processes, persistent delusions or hallucinations, disorientation, memory loss of close relatives or one’s own name, or inability to perform activities of daily living. |
$3,831.30/month |
Compensation amounts are sourced from the VA’s current Disability Compensation Rates on VA.gov (effective December 1, 2024).
Example: A veteran reporting “occasional nightmares” with stable work may receive 30%. Another who cannot maintain employment, isolates socially, and experiences daily panic may qualify for 70% or 100%.
Your C&P exam for PTSD heavily influences this rating. During the exam, the VA examiner assesses your mental health symptoms and records them on the Disability Benefits Questionnaire (DBQ). And this documentation of symptoms by the examiner on the PTSD DBQ, especially under “Occupational and Social Impairment” is the single most important factor in determining your percentage.
Common Secondary Conditions to PTSD
PTSD can lead to a wide range of secondary conditions recognized by the VA. These include:
- Major Depressive Disorder (MDD): Depression frequently overlaps with PTSD symptoms such as hopelessness, isolation, and lack of motivation.
- Anxiety Disorders: Veterans may experience panic attacks and hypervigilance, both of which are often noted during a PTSD C&P exam.
- Substance Use Disorders: Many veterans turn to alcohol or drugs to cope, which the VA may consider service-connected if secondary to PTSD (Allen v. Principi, 2001).
- Migraines and Chronic Pain: Stress and poor sleep quality from PTSD often manifest as headaches or muscle tension.
- Cardiovascular Conditions: Research shows that prolonged stress and hyperarousal increase risks for hypertension and heart disease.
If these conditions are caused or worsened by PTSD, they may qualify for secondary service connection.
During a DBQ for PTSD or a VA mental health C&P exam, examiners will document these comorbidities if present. Veterans should openly discuss all symptoms since secondary conditions can significantly increase overall ratings.
PTSD, Occupational Impairment, and TDIU
VA ratings for PTSD range from 0% to 100%, but many veterans fall in the 50–70% range. At these levels, symptoms often include difficulty maintaining relationships, problems with authority, chronic sleep impairment, and impaired judgment. These limitations may prevent steady employment.
This is where TDIU (Total Disability based on Individual Unemployability) protects a veteran’s compensation. Even if a veteran’s PTSD is rated at 70%, TDIU allows them to be compensated at the 100% rate if the condition prevents them from securing and maintaining gainful employment.
For example, a combat veteran with a 70% PTSD rating who also suffers from migraines and alcohol dependency might struggle to hold a steady job. With supporting medical evidence, often strengthened by a PTSD DBQ and lay statements, the veteran may qualify for TDIU.
7 Essential Tips for Your VA PTSD C&P Exam
Being fully prepared for the Compensation and Pension exam often determines whether VA fully understands the impact of your condition. Here are important PTSD C&P exam tips to help you succeed and ensure a smoother path to deserved benefits.
1. Write Down Your Symptoms
It’s easy to forget details under stress. Before the VA PTSD examination, create a symptom diary covering nightmares, irritability, avoidance behaviors, and concentration problems. Veterans often tell me they “go blank” at the moment, your notes will prevent this.
2. Bring Supporting Evidence
If you have treatment records, therapy notes, or a favorable medical opinion, bring them. Even though examiners should review your file, they may overlook key documents. A DBQ for PTSD increase from a private provider can strengthen your claim.
3. Bring a Witness if Possible
A spouse or close friend can describe how PTSD affects your daily functioning. Even if they aren’t allowed in the exam room, their written statement may be valuable.
4. Stay Aware of Examiner Observations
Remember, you are being evaluated from the moment you step into the waiting room. A VA mental health C&P examiner may note your mood, grooming, or body language. If your PTSD affects daily hygiene, sleep, or social interactions, be open about it, as these details often shape the final report.
5. Be Honest and Specific
Don’t minimize symptoms (“I’m fine”) or exaggerate. Focus on your worst days. For example, explain how panic attacks kept you from holding a steady job.
6. Expect Common Questions
Examiners may ask about your military stressor, flashbacks, and social/occupational impairment. Review the VA PTSD C&P exam questions so you’re not caught off guard.
7. Document What Happens After
Take notes about the exam length, examiner’s behavior, and whether you felt heard. If your claim is denied, this record can help challenge the results.
Disclaimer: This article is for general information only and is not medical, psychological, or legal advice. Always verify details on VA.gov and consult a licensed clinician or a VA-accredited representative about your specific situation.
If you’re in crisis or thinking about self-harm: Contact the Veterans Crisis Line—call or text 988 then Press 1, chat at VeteransCrisisLine.net/chat, or dial 711 then 988 for TTY. If you’re in immediate danger, call 911.
The Path Forward
Once the C&P exam is complete, the examiner compiles all the information and sends the DBQ back to the VA. The adjudicator then reviews the findings, considering the checked blocks that correspond to specific ratings. The decision-making process involves determining the relationship between the condition and military service and assigning a disability percentage based on the severity of the symptoms.
In navigating the C&P exam for PTSD, honesty, preparation, and understanding the evaluation criteria are key elements for veterans seeking fair and accurate disability ratings. By actively participating in the process and providing transparent information, veterans can contribute to a more comprehensive assessment of their PTSD and receive the support they deserve.
FAQs
What to say to get 70% PTSD compensation?
To qualify for a 70% PTSD rating, describe to the examiner severe symptoms like:
- Suicidal thoughts
- Near-continuous panic or depression
- Impaired impulse control
- Neglect of hygiene, or
- Inability to handle stress that causes major work and social impairment
Does the VA always use DSM-5?
Yes, VA examiners use DSM-5 criteria during PTSD C&P exams to confirm diagnosis, symptoms, and severity.
What is VA Form 21-0781?
VA Form 21-0781 is used to document your in-service PTSD stressor events.
What if I disagree with my rating?
If you disagree with your PTSD rating after a C&P exam, you can challenge it by filing a Supplemental Claim, requesting a Higher-Level Review, or appealing to the Board of Veterans’ Appeals.
Can PTSD be secondary to another condition?
Yes, PTSD can be secondary to or cause secondary conditions such as depression, anxiety, migraines, or substance use, which may increase your overall VA rating.
What are the criteria for PTSD diagnosis?
The DSM-5 criteria for PTSD require trauma exposure, re-experiencing, avoidance, negative mood changes, hyperarousal, symptoms lasting over one month, and significant life impairment not due to substances or another condition.
What mental health tests are used during a PTSD C&P exam?
- Clinician-Administered PTSD Scale for DSM-5 (CAPS-5)
- Beck Depression Inventory (BDI)
- PTSD Checklist for DSM-5 (PCL-5)
- Minnesota Multiphasic Personality Inventory-2 (MMPI-2)
- Personality Assessment Inventory (PAI)
What do I need to prove PTSD to the VA?
You must show a current PTSD diagnosis, an in-service stressor event, and medical evidence linking your symptoms to that service.
What qualifies as combat PTSD?
Combat PTSD is diagnosed when a veteran develops PTSD symptoms after direct exposure to traumatic combat events such as firefights, IED blasts, or witnessing death in service.
Also read: Proposed New Rules for PTSD VA Compensation
At Prestige Veteran Medical Consulting, a veteran-owned company, we specialize in Independent Medical Opinions (IMOs) known as Nexus letters.
Our purpose is to empower YOU, the veteran, to take charge of your medical evidence and provide you with valuable educational tools and research to guide you on your journey.
Understanding the unique challenges veterans face, our commitment lies in delivering exceptional service and support.
Leveraging an extensive network of licensed independent medical professionals, all well-versed in the medical professional aspects of the VA claims process, we review the necessary medical evidence to incorporate in our reports related to your VA Disability Claim.
Prestige Veteran Medical Consulting is not a law firm, accredited claims agent, or affiliated with the Veterans Administration or Veterans Services Organizations. However, we are happy to discuss your case with your accredited VA legal professional.













