Last Updated on 8 August, 2025
Reviewed by: A former U.S. military veteran from Prestige Veteran Medical Consulting Services, experienced in helping veterans navigate VA claims and secure compensation.
Traumatic Brain Injury (TBI) is a significant concern for veterans, particularly those who have experienced combat or high-risk training environments. This blog offers an in-depth analysis of TBI, its symptoms, VA disability ratings, and how veterans can enhance their chances of receiving the benefits they deserve. If you or a loved one from military service has suffered from a TBI, understanding the VA claims process and available compensation is crucial.
Table of Contents
What is Traumatic Brain Injury in Veterans?
Traumatic Brain Injury (TBI) is a condition occurring when an external blow or jolt to the head, penetration of an object into the skull, or forces generated by blasts and explosions disrupt normal brain function.
These brain injuries range from mild (commonly referred to as concussions) to moderate and severe. TBIs affect brain function and can result in physical, cognitive, and emotional impairments. Veterans are at an increased risk of traumatic brain injury due to their exposure to combat, IED blasts, training exercises, and hazardous environments.
According to the Department of Defense’s Traumatic Brain Injury Center of Excellence, a total of 515,885 service members were diagnosed with TBI between 2000 and 2024.
The Department of Veterans Affairs (VA) recognizes traumatic brain injury as a significant disability and offers compensation based on the severity of its residual effects.
Common Causes of TBI in Veterans
Around 20% of post-9/11-era military veterans who served in the Iraq and Afghanistan wars sustained a traumatic brain injury during their deployment, according to data from the VA and the Department of Defense.
Service members typically may experience TBIs in various ways, including:
- Explosions from Improvised Explosive Devices (IEDs)
- Combat-related head trauma
- Motor vehicle accidents
- Falls during training or operational activities
- Personal assaults or military sexual trauma
Symptoms of Traumatic Brain Injury
TBI is often called an “invisible injury” because symptoms like headaches, memory loss, mood changes, and sleep problems aren’t physically visible. Some TBI symptoms appear immediately, while others develop over time, for example,
Immediate Symptoms
- Confusion or disorientation
- Seeing “stars”
- Dizziness or balance issues
- Loss of consciousness or being “knocked out”
- Headaches
- Memory loss surrounding the incident
Long-Term Symptoms
- Persistent headaches or neck pain
- Sensitivity to light and noise
- Cognitive dysfunction (difficulty concentrating, poor memory, slow processing)
- Mood swings, depression, anxiety, or impulsiveness
- Speech and communication difficulties
- Sleep disturbances
- Seizures or neurological deficits
- Changes in social behavior, including isolation or aggression
Mild, Moderate, and Severe TBI
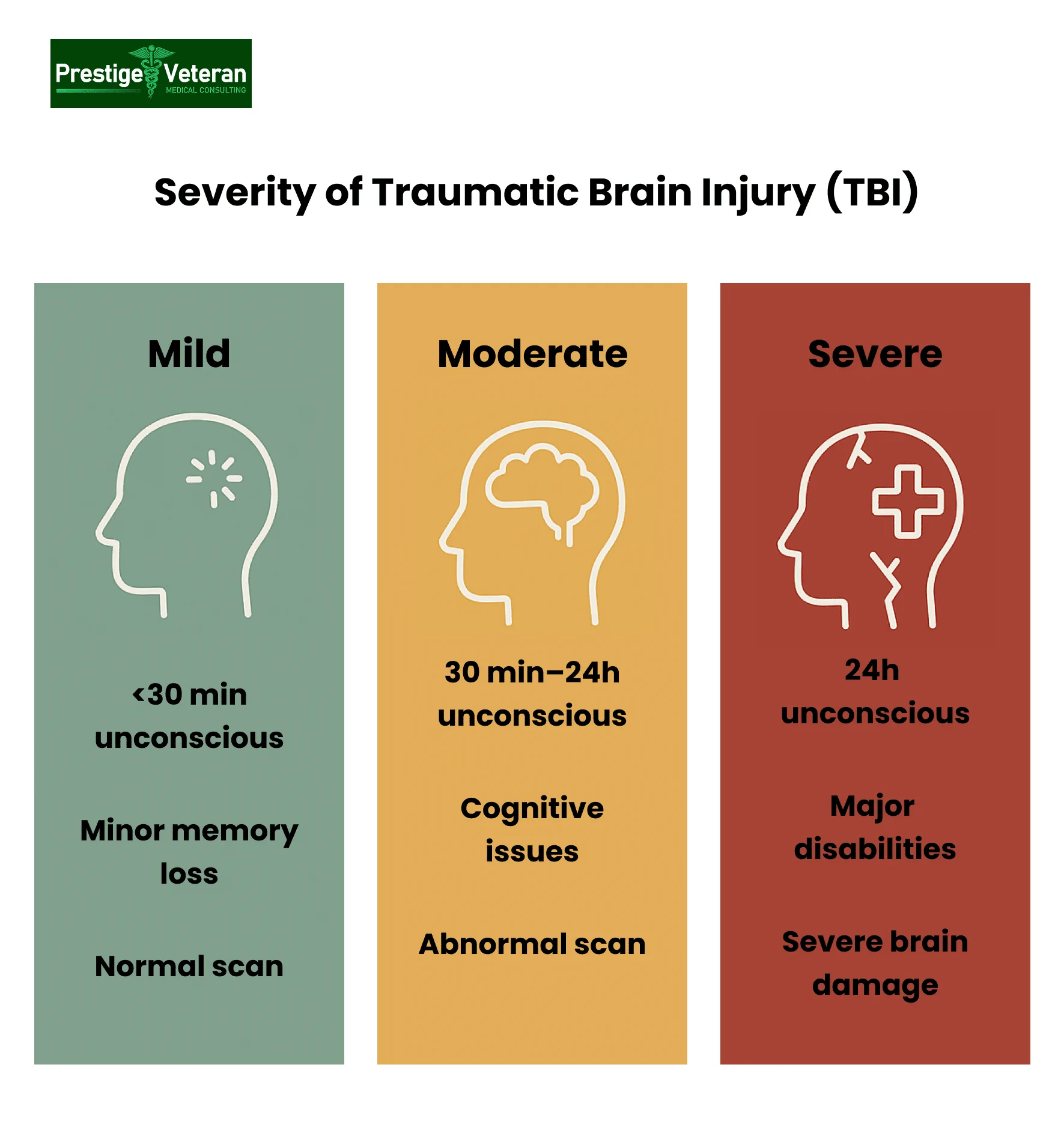
The VA classifies traumatic brain injuries based on the Glasgow Coma Scale, duration of unconsciousness, memory loss, and brain imaging results:
- Mild TBI (Concussion): Loss of consciousness for under 30 minutes, minor memory loss, and normal brain imaging.
- Moderate TBI: Unconsciousness lasting 30 minutes to 24 hours, notable cognitive impairment, and abnormal imaging.
- Severe TBI: Loss of consciousness for over 24 hours, significant cognitive and physical disabilities, and serious neurological damage.
TBI-Related Medical Conditions
Many veterans with traumatic brain injuries experience medical complications that can directly influence VA disability ratings. For instance,
- Concussions: Mild brain trauma often overlooked in combat situations.
- Edemas: Swelling in the brain that can increase pressure and cause further injury.
- Hematomas: Blood clots in or around the brain requiring urgent care.
- Diffuse Axonal Injury: Widespread nerve damage from rapid head movement or blast waves.
- Skull Fractures: Breaks in the skull that may lead to brain tissue damage.
- Contusions: Bruising of brain tissue, often from direct blows.
Accurate diagnosis is vital, as these conditions can cause lasting impairments that limit daily function and employability, qualifying for increased VA benefits.
VA TBI Screening for Veterans
Veterans who believe they may have suffered a Traumatic Brain Injury during service undergo a mandatory screening through the VA, especially if they were never formally diagnosed but now experience symptoms like memory loss, headaches, or mood changes.
The process begins with a 4-question screening questionnaire at a VA facility. If results indicate possible TBI, the veteran is referred for a comprehensive evaluation, including neurological exams, cognitive testing, and a review of service history.
In a 2025 study, about 1 in 4 U.S. veterans screened positive for probable TBI, which was linked to higher rates of physical, mental, and cognitive health issues.
Early TBI screening helps veterans access treatment, establish service connection, and file a VA disability claim for related conditions. Contact your local VA to begin the process.
Treatment Options
Treatment of traumatic brain injuries focuses on healing the brain and managing symptoms with therapy, medication, and lifestyle changes. Depending on severity, TBI patients can recover through physical therapy, speech therapy, or cognitive rehabilitation to restore daily function.
Gaining VA benefits for TBI provides veterans access to specialized care, treatment, rehabilitation, and financial compensation for service-connected injuries.
VA Disability Rating for TBI
The VA disability rating for TBI determines how much monthly compensation a veteran receives for service-connected traumatic brain injury. Understanding the rating criteria and evaluation process ensures veterans receive the VA benefits they have earned.
How the VA Rates TBI
The VA rates TBI using Diagnostic Code 8045 under 38 CFR § 4.124a. Unlike many other disabilities, TBI is rated based on its residual effects rather than the initial severity of the injury. The key areas of ongoing impairment on which VA TBI ratings are based are:
- Cognitive – problems with memory, attention, concentration, and executive functions.
- Emotional/behavioral – mood or personality changes (when not separately rated under a mental disorder code).
- Physical/neurological – motor or sensory loss, headaches, balance problems, speech issues, etc.
To measure cognitive and other residuals, VA uses the “Evaluation of Cognitive Impairment and Other Residuals of TBI Not Otherwise Classified” table. This table assigns a severity value of 0, 1, 2, 3, or “total” impairment to each of the ten facets of TBI-related dysfunction, which correspond to a disability percentage:
- Memory, Attention, Concentration, Executive Functions
- Judgment
- Social Interaction
- Orientation
- Motor Activity
- Visual-Spatial Orientation
- Subjective Symptoms (e.g., headaches, dizziness, tinnitus)
- Neurobehavioral Effects (e.g., mood swings, aggression)
- Communication
- Consciousness (e.g., coma or vegetative state)
If a veteran has a “total” impairment rating in any facet, they receive 100% VA disability benefits for TBI.
Note: Per the Federal Register (Nov. 12, 2024), VA adjudicators must consider all three domains—cognitive, emotional/behavioral, and physical- when applying DC 8045 and avoid “pyramiding” if symptoms overlap with other service-connected conditions like PTSD or migraines.
TBI VA Disability Rating Scale
Below is the VA TBI disability percentage chart under Diagnostic Code 8045, showing how severity values correspond to compensation levels:
|
VA TBI Facet |
0 (0%) |
1 (10%) |
2 (40%) |
3 (70%) |
Total (100%) |
|
Memory, Attention, Concentration, Executive Functions |
No impairment |
Mild difficulty; no interference with work |
Moderate issues; some interference with work/daily life |
Severe impairment; needs assistance for daily activities |
Complete inability to perform these functions |
|
Judgment |
Normal decision-making |
Mildly impaired judgment |
Often makes poor decisions |
Consistently unsafe decisions |
Completely unable to make decisions |
|
Social Interaction |
Always appropriate |
Occasionally inappropriate |
Frequently inappropriate |
Always inappropriate |
Cannot interact socially |
|
Orientation |
Fully oriented |
Occasionally disoriented |
Often disoriented |
Consistently disoriented |
Completely unaware of self or surroundings |
|
Motor Activity |
Normal motor control |
Mild slowing or clumsiness |
Moderate loss of coordination/movement |
Severe loss; needs assistance |
Complete inability to move voluntarily |
|
Visual-Spatial Orientation |
Normal spatial awareness |
Mild difficulty judging space/distance |
Gets lost in familiar places |
Cannot navigate even in familiar areas |
Complete inability to orient in space |
|
Subjective Symptoms |
No symptoms |
Mild, occasional symptoms (e.g., headaches, dizziness) |
Frequent symptoms that interfere with work |
Severe symptoms that significantly limit activity |
Totally incapacitating symptoms |
|
Neurobehavioral Effects |
No mood or behavior issues |
Mild, occasional issues (e.g., irritability, apathy) |
Interferes with work or relationships |
Requires supervision for safety |
Cannot manage own behavior |
|
Communication |
Normal communication |
Mild word-finding or comprehension issues |
Frequent difficulty understanding or expressing |
Severe impairment; needs alternative communication |
Complete inability to communicate |
|
Consciousness |
Normal consciousness |
— |
— |
— |
Coma, vegetative state, or minimal consciousness |
TBI Rating Criteria Explained
- 0% Rating: A Traumatic Brain Injury is diagnosed, but symptoms do not significantly impact daily life.
- 10% Rating – Mild symptoms like occasional headaches, slight memory loss, and mild difficulty with judgment.
- 40% Rating – Moderate symptoms like impaired judgment, moderate memory loss, and difficulty in performing work and daily activities.
- 70% Rating – Severe symptoms causing social isolation, disorientation, severe memory loss, inability to make decisions without assistance, and major impairments.
- 100% Rating – Total cognitive dysfunction, requiring constant assistance.
Veterans may also be eligible for Special Monthly Compensation (SMC-T) if they require aid and attendance due to severe TBI.
The Link Between TBI and Mental Health Conditions
TBI and PTSD
Traumatic Brain Injury (TBI) and Post-Traumatic Stress Disorder (PTSD) often occur together in veterans, particularly those exposed to combat-related blasts. A 2025 Defense Health Agency report found that individuals with probable TBI are more likely to have post-traumatic stress disorder (PTSD), with 27.6% affected compared to just 4.1% of those without the injury.
While PTSD symptoms primarily affect emotional and behavioral health, TBI adds physical and cognitive impairments such as memory loss, dizziness, poor judgment, and difficulty concentrating. The VA rates TBI and PTSD separately if their symptoms are distinct; however, overlapping symptoms (e.g., anxiety, depression, or sleep disturbances) may result in a single combined rating to prevent pyramiding.
TBI and Other Mental Health Conditions
Beyond PTSD, traumatic brain injuries have been linked to other mental disorders like major depressive disorder, generalized anxiety disorder, dementia, and other conditions. The VA prohibits “pyramiding” (rating the same symptoms under multiple conditions), meaning a veteran rated for depression under TBI criteria cannot receive a separate depression rating. However, PTSD, migraines, and some neurological disorders may be rated separately if they have distinct symptoms.
Veterans with TBI-related mental health conditions should establish potential secondary claims to maximize VA disability benefits.
Understanding TBI and Migraines
Chronic headaches and migraines are among the most common residuals of TBI. A 2022 study published in ScienceDirect found that approximately 75% of individuals with mild traumatic brain injury developed post-traumatic headaches, with many experiencing frequent or migraine-like symptoms.
Unlike Parkinson’s disease, seizures, and some types of dementia, which are considered presumptive conditions of TBI, migraines are not automatically recognized as a secondary condition.
However, the VA recognizes migraines as a separate condition rated under 38 CFR § 4.124a, Diagnostic Code 8100, offering disability ratings from 0% to 50% based on severity and frequency. Veterans suffering from both TBI and migraines can receive compensation for each, as migraines qualify under distinct diagnostic criteria.
Severe, prostrating migraines can also contribute to Total Disability Individual Unemployability (TDIU) eligibility, ensuring veterans unable to maintain gainful employment due to TBI-related symptoms receive full benefits.
Is VA Disability for Traumatic Brain Injury (TBI) Presumptive?
While TBI itself is not classified as a presumptive disability, VA regulations enacted in January 2014 have recognized that moderate or severe service-connected TBIs can lead to certain secondary conditions that are presumed to be connected to military service.
Under 38 CFR § 3.310(d), five conditions qualify for presumptive service connection when they develop within specific timeframes following a qualifying TBI:
- Parkinson’s Disease – any time after moderate or severe TBI
- Seizures – any time after moderate or severe TBI, with no other cause
- Dementia – if diagnosed within 15 years of moderate or severe TBI
- Depression – within 3 years of moderate/severe TBI or 1 year after mild TBI
- Hormonal Imbalance – within 1 year of moderate or severe TBI
To qualify, the original TBI must be service-connected and classified by severity determined through imaging, duration of unconsciousness, altered mental status, or Glasgow Coma Scale. This means that veterans must still prove a service connection through a current diagnosis of TBI, in-service injury, and a medical nexus linking the two.
Eligibility for VA TBI Presumptive Conditions:
- Confirm TBI is service-connected
- Verify diagnosis of presumptive condition
- Ensure it falls within the required time window
- Rule out other causes for the secondary condition
This presumption removes the burden of proving a direct causal link between TBI and its residual conditions, making it easier to obtain VA disability compensation.
How Can Veterans Secure a Favorable TBI VA Rating
Receiving a fair VA disability rating for a traumatic brain injury (TBI) requires thorough documentation and a well-supported claim. Below are key strategies that can strengthen your case:
1. Document Your TBI Diagnosis
- Obtain a formal medical diagnosis from a VA neurologist or private healthcare provider.
- Keep records of medical treatments, diagnostic imaging (MRIs, CT scans), neuropsychological tests, and cognitive evaluations.
2. Gather Evidence of In-Service Incident of the TBI Event
- Compile service treatment records detailing head injuries or hazardous exposure during combat.
- Obtain lay statements from fellow service members, supervisors, or family members who firsthand observed your symptoms post-injury.
- Deployment records (DD214 copies) or combat history can further validate events that caused the TBI, e.g. IED blasts, training injury, motor vehicle accident, etc.
Download VA Form 21-4138 (PDF) – Statement in Support of Claim
3. Establish a Medical Nexus
A nexus letter from a qualified neurologist or physician helps prove that your TBI is “at least as likely as not” connected to your military service. This expert opinion should include details on how the brain injury affects cognitive, emotional, and physical functions. The nexus letter doctor should provide medical reasoning backed by diagnostic findings, linking the condition to service-related events.
A well-written nexus statement increases the chances of claim approval, as it serves as expert testimony connecting your TBI to military duty. Prestige Veteran Medical Consulting provides expert independent medical opinions to help veterans establish evidence-backed service connection to increase their benefits.
4. File for Secondary Service-Connected Conditions
Veterans with TBI can secure a higher VA rating by filing for secondary service-connected conditions or residuals of TBI. Here’s a list of common secondary conditions many veterans face:
- Post-Traumatic Stress Disorder (PTSD)
- Depression and anxiety
- Parkinson’s disease
- Dementia
- Unprovoked seizures
- Migraine headaches
- Sleep disorders (e.g., sleep apnea)
- Hormone deficiencies
- Chronic Fatigue Syndrome
- Chronic pain
- Dizziness or balance problems
- Vision problems
- Tinnitus or hearing loss
- Speech or language difficulties
- Motor or sensory impairments
Obtaining service connection for secondary claims often increases overall VA disability compensation, ensuring veterans receive the benefits they deserve for conditions caused by their service-related TBI.
5. Identify TBI Residuals to Be Rated Separately
To maximize your TBI VA rating, it’s crucial to identify residual conditions, such as migraines, PTSD, depression, or tinnitus, that may warrant separate ratings. While TBI is rated under Diagnostic Code 8045, covering 10 functional areas, some TBI residuals qualify for higher ratings under different codes.
For example, migraines (DC 8100) can be rated up to 50%, PTSD (DC 9411) up to 100%, and tinnitus (DC 6260) at 10%. If a TBI residual is more severe and independently ratable, request evaluation under the more favorable code to avoid “pyramiding” and ensure you yield a higher combined VA disability rating.
You may speak with a Veterans Service Organization (VSO) or an accredited VA representative on filing a VA claim for TBI or residuals.
6. Attend Your Compensation & Pension (C&P) Exam
The VA may schedule a Compensation & Pension (C&P) exam for veterans seeking VA disability benefits. Conducted by VA-approved medical professionals, this exam determines the severity of a service-related TBI and assesses its lasting impact on daily life.
If a mental health condition is claimed as a secondary service connection for TBI, the examiner must follow the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5) assessments to ensure an accurate diagnosis and rating.
During the TBI C&P exam, the examiner will:
- Review medical history, including service treatment records and prior diagnoses.
- Conduct a physical and neurological examination to assess symptoms.
- Evaluate symptoms like cognitive function, memory, concentration, motor skills, and behavioral changes.
- Perform imaging tests such as CT scans or MRIs if necessary.
The C&P exam findings influence the VA disability rating, which ranges from 0% to 100% based on the severity of TBI residuals (e.g., memory loss, headaches, and mood disorders). Veterans should thoroughly document their symptoms and bring a caregiver or witness if memory issues affect their ability to communicate.
These Compensation & Pension exam results may impact your final VA rating; hence, failing to attend it can even result in a denied claim.
Tip: If possible, have a VA TBI DBQ completed from your provider before your C&P exam to strengthen your claim with consistent, detailed findings.
7. Consider Applying for TDIU Benefits
If your TBI symptoms prevent you from maintaining substantially gainful employment, you may qualify for Total Disability Individual Unemployability (TDIU) benefits.
For example, a veteran may receive a 100% VA rating if they experience severe cognitive dysfunction, total physical disability, or frequent loss of consciousness. TDIU allows veterans to receive 100% disability compensation even if their official VA rating is below 100%.
Eligibility Criteria for TDIU:
- One service-connected disability rated at 60% or higher, OR
- Two or more service-connected disabilities with a combined rating of 70%, with one disability rated at least 40%.
TDIU for traumatic brain injuries is crucial for veterans whose symptoms make it impossible to hold a steady job but who do not meet the standard 100% disability rating.
8. Track Changes in TBI Symptoms for Re-Evaluation
TBI symptoms often change or worsen over time. Veterans should document new or increased issues like memory loss, headaches, or mood changes, attend all C&P exams, and request a re-evaluation when needed. Keeping detailed medical records ensures your TBI VA rating stays accurate and reflects the true impact on your daily functioning.
70% Disability Rating for TBI: Special Considerations
A 70% VA disability rating for TBI indicates that a veteran is experiencing significant cognitive, emotional, or physical impairments. These can include:
- Severe memory loss
- Social isolation
- Disorientation
- Frequent headaches
- Poor judgment
- Neurobehavioral issues like physical aggression or emotional instability
At this level, a veteran may struggle with maintaining substantially gainful employment and daily functioning but does not yet qualify for a total disability rating.
A veteran should ensure that their neurobehavioral symptoms and cognitive impairments are thoroughly documented. Additionally, secondary conditions like PTSD, migraines, or seizures often develop from TBI, and failing to claim them could mean missing increased benefits.
Oftentimes, the VA may underestimate the severity of your condition. Keep detailed service records, obtain a strong medical nexus letter, and consider applying for TDIU benefits if you cannot work due to the traumatic brain injury.
Special Monthly Compensation (SMC) for Severe TBI
Veterans with severe TBI may qualify for Special Monthly Compensation (SMC-T) if they require aid and attendance. This benefit provides additional financial support beyond the standard disability rating. Even if a veteran is rated at 100 percent for service-connected TBI, they would still receive additional compensation for SMC.
Signs You’re Eligible for SMC-T
- You have a service‑connected TBI.
- You need regular aid and attendance (bathing, dressing, feeding, or maintaining hygiene) due to TBI.
- Without in-home care, you would require nursing home or institutional care.
- You do not qualify for a higher level of aid and attendance (SMC-R2).
If you meet all four criteria, you may qualify for Special Monthly Compensation.
2025 SMC Payment Amounts
A veteran requiring aid and attendance for severe TBI may qualify for Special Monthly Compensation (SMC‑T). For a single veteran alone, the 2025 SMC‑T monthly rate is $10,964.66.
Higher payment rates apply when dependents are included; for example, a veteran with a spouse and two dependent parents can receive up to $11,521.15 per month.
SMC vs. TDIU Differences
- TDIU grants compensation at the 100% disability rating, but is capped at the standard payment (e.g., about $3,831 monthly for a single veteran TBI at 100%)
- SMC‑T, in contrast, replaces, not adds to, a veteran’s monthly disability compensation, and offers a much higher, care‑based benefit.
How to File a TBI VA Disability Claim
Many Veterans follow these steps to file a TBI disability claim and ensure fair compensation:
- Gather Medical Evidence: Obtain a confirmed TBI diagnosis, military service records, nexus letters, and buddy statements.
- File Your Claim Online or In-Person: Use VA.gov or visit a VA regional office. Additionally, consider consulting an accredited legal professional for assistance when needed.
- Attend the C&P Exam: Ensure your symptoms are thoroughly documented.
- Await a Decision: The VA will notify you of your rating.
- File an Appeal if Necessary: If your TBI VA rating is too low, consider an appeal with legal assistance.
Disability Benefits Questionnaire (DBQ) for TBI VA Claims
The VA’s Traumatic Brain Injury (TBI) Disability Benefits Questionnaire (DBQ) provides a structured medical assessment that can impact a veteran’s rating and compensation. It documents the severity of residual effects across ten functional facets, such as memory, judgment, motor activity, and neurobehavioral changes.
The VA TBI DBQ form is used during Compensation & Pension (C&P) exams or by private specialists to prove service connection, secondary conditions, and eligibility for higher ratings or Special Monthly Compensation (SMC-T).
For example, a well-prepared DBQ for VA TBI may help separate TBI symptoms from overlapping PTSD to avoid reduced ratings and ensure maximum compensation for service-connected brain injuries.
Top Mistakes Veterans Make with TBI VA Claims (and How to Avoid Them)
Whether you’re seeking a VA TBI rating of 40 percent, 70 percent, or even 100 percent through TDIU or SMC, avoiding these common errors can increase your chances of securing claim approval and fair compensation.
Mistake 1: Not Separating TBI and PTSD Symptoms
One of the most common and costly mistakes is failing to differentiate between symptoms of TBI and PTSD. Because these conditions often share similar manifestations, such as memory loss, irritability, sleep disturbances, or depression, the VA may combine their ratings to avoid “pyramiding“. This can significantly reduce your traumatic brain injury VA rating and compensation.
Tip: Ask your doctor or specialist to clearly separate symptoms for each condition in your VA TBI DBQ or private records.
2. Skipping a Medical Nexus Letter
Failing to submit a nexus letter in your TBI VA disability claim can be a huge mistake. Without it, the VA often lacks enough medical evidence to grant service connection for your traumatic brain injury VA claim. Even worse, a vague or poorly written medical nexus letter that doesn’t clearly state that TBI is “at least as likely as not” linked to military service can be just as damaging.
Tip: For example, a veteran injured in a convoy blast might use deployment records, MRI reports, and a neurologist’s opinion to strengthen the link, securing a favorable rating under 38 CFR TBI regulations.
3. Not Claiming Secondary Conditions
TBI VA disability often results in other debilitating conditions such as migraines, depression, seizures, or hormonal imbalances. Veterans frequently forget to claim these secondary conditions, leaving money and benefits on the table.
Tip: The VA recognizes five presumptive conditions related to moderate or severe TBI, including Parkinson’s and dementia. Don’t forget to file them in your VA disability for TBI claim.
4. Underreporting Symptoms During C&P Exams
Veterans often downplay symptoms or forget to report cognitive impairments during the Compensation & Pension (C&P) exam. This mistake in your claim can lead to a lower VA TBI rating.
Tip: Keep a daily symptom journal and bring a witness to help communicate issues like disorientation or communication problems.
5. Ignoring Favorable Diagnostic Codes
The VA is required to rate your condition under the code that yields the highest benefit. If migraines or depression caused by TBI offer a higher rating than the TBI VA rating criteria under DC 8045, the VA must rate accordingly. Veterans unaware of this rule miss the chance to maximize disability benefits.
Tip: Ask your doctor to use the diagnostic code that offers the highest VA TBI rating based on your symptoms.
6. Relying Solely on VA Medical Records
Many veterans depend solely on VA doctors who might not fully document their TBI residuals or understand their condition. This TBI VA claim mistake can result in a lower disability rating.
Tip: Private neurologists, psychologists, or TBI specialists often provide more detailed assessments, especially if you’re seeking a VA TBI rating of 70 percent or higher. Submitting independent medical opinions can tip the scales in your favor.
Studying a Real-Life VA Disability Case for TBI
A post-9/11 combat veteran (Iraq, 2008–2011) appealed for higher VA disability ratings and earlier effective dates for Traumatic Brain Injury, headaches with photophobia, and tinnitus.
The Board of Veterans’ Appeals confirmed a 70% rating for TBI, based on moderate cognitive impairment, such as memory loss, impaired concentration, poor judgment, and communication difficulty, but found no evidence of “total” impairment to justify a 100% rating.
VA Disability Ratings Awarded:
- TBI: 70% (confirmed)
- Headaches with Photophobia:
- 0% from March 8, 2011, to March 1, 2015
- 30% from March 2, 2015 (due to prostrating attacks)
- Tinnitus: 10% (maximum allowed)
The VA denied earlier effective dates, setting the claim start as March 8, 2011, the day after discharge. However, the Board granted TDIU from February 12, 2012, recognizing that TBI and PTSD symptoms (already rated at 50%) prevented the veteran from securing gainful employment.
Key Evidence Supporting the Decision:
- May 2012 and March 2015 VA examinations showing moderate cognitive impairment
- Documented residuals like memory, attention, and judgment deficits
- Neurobehavioral symptoms like irritability and poor social interaction
- VA examiner’s medical opinion linking PTSD and TBI to unemployability
- Unemployability evidence indicating that the veteran had not worked since February 2012
The Board additionally remanded the claim for Special Monthly Compensation (SMC) under 38 U.S.C. § 1114(s) to determine if TDIU was based on a single disability and if another separate service-connected condition rated 60% or more existed (Bradley v. Peake).
This case highlights how important documenting medical evidence and symptoms is for securing a high VA disability rating for a TBI claim.
Board of Veterans’ Appeals, Citation No. 1608951 (Mar. 7, 2016).
2025 VA TBI Disability Rating Compensation Chart
The 2025 VA TBI pay rates determine how much monthly compensation a veteran with a Traumatic Brain Injury disability rating receives. These VA disability compensation rates are based on the percentage rating assigned by the Department of Veterans Affairs and are updated annually to reflect cost-of-living adjustments (COLA).
Below is the full VA TBI disability pay chart for 2025, showing monthly payments for a single veteran.
| VA Disability Rating Percentage | Monthly Payment (Single Veteran) |
| 0% | $0.00 |
| 10% | $175.51 |
| 20% | $346.95 |
| 30% | $537.42 |
| 40% | $774.16 |
| 50% | $1,102.04 |
| 60% | $1,395.93 |
| 70% | $1,759.19 |
| 80% | $2,044.89 |
| 90% | $2,297.96 |
| 100% | $3,831.30 |
Note: Additional compensation is available for eligible dependents if your disability rating is 30% or higher. For example, a veteran with a 50% VA TBI rating who has a spouse and one child could receive $1,287.04 per month in 2025 instead of the base $1,102.04 rate for veterans with no dependents.
How to Appeal a Denied TBI Claim
Unfortunately, the VA frequently underrates TBI claims or denies them due to a lack of medical evidence. If you receive an unfair rating, you have the right to appeal the decision per the Appeals Modernization Act (AMA).
Options to Appeal an Unfavorable TBI Claim (according to VA.gov):
- Request a Higher-Level Review: Have a senior VA examiner reassess your claim.
- Submit a Supplemental Claim: Provide new medical evidence to strengthen your case.
- Appeal to the Board of Veterans’ Appeals: If previous appeals fail, you can escalate your case to a Veterans Law Judge.
Working with a VA-accredited attorney, claims agent, or Veteran Service Organizations (VSOs) can improve your chances of success, as they understand how to navigate complex VA regulations.
Conclusion
Traumatic Brain Injury is a serious condition affecting thousands of veterans. Understanding the VA TBI rating process, documenting symptoms, and pursuing secondary conditions can significantly increase a veteran’s disability rating and benefits. Veterans should take advantage of VA resources and legal assistance to ensure they receive the compensation they deserve. Your service matters, and so does your compensation.
Disclaimer: This article is for informational purposes only and does not constitute legal or medical advice. Please consult a VA-accredited attorney or representative for personalized guidance.
FAQs
What is the average VA rating for TBI?
The average VA rating for traumatic brain injury varies but often falls between 40% and 70%, depending on documented residual effects.
How to get a 70% rating for TBI?
To receive a 70% TBI VA rating, a veteran must demonstrate that their symptoms align with Level 3 severity on the VA’s cognitive impairment scale, including major memory loss, disorientation, total social and occupational impairment, or neurobehavioral issues affecting daily life.
How do I prove my TBI claim to the VA?
You need a formal TBI diagnosis, service records showing the injury, a nexus letter, which may be helpful in linking it to service, and documented residual symptoms supported by medical evidence.
How do I increase my TBI VA rating?
To increase VA ratings for traumatic brain injury, veterans can document worsening of symptoms, file for secondary conditions (e.g., PTSD, migraines, seizures), request a higher-level review, or consider Total Disability Individual Unemployability (TDIU) if unable to work.
Is TBI a presumptive condition?
TBI itself is not automatically presumptive, but it can lead to other service-connected conditions (e. g. Parkinson’s disease, dementia, and seizures) that may be considered presumptive after moderate or severe TBI.
How to get a 100% VA disability rating for TBI?
A 100% VA rating for TBI requires proof of “total” impairment in at least one rating facet, such as complete cognitive dysfunction, under Diagnostic Code 8045.
Can VA perform a test for TBI?
Yes, the VA conducts a mandatory TBI screening and, if positive, follows up with comprehensive neurological and cognitive evaluations.
What are 5 symptoms of TBI?
Common TBI symptoms include memory loss, headaches, dizziness, mood changes, and difficulty concentrating.
How does the VA rate TBI when migraines are involved?
TBI and migraines can be rated separately if symptoms are distinct, with migraines rated up to 50% under Diagnostic Code 8100.
What is the VA disability rating scale for TBI?
The VA rates TBI residuals from 0% to 100% based on impairment severity across ten functional areas, from mild symptoms to total cognitive dysfunction.
Can veterans receive a Purple Heart for a traumatic brain injury (TBI)?
Yes, veterans may be awarded a Purple Heart for a TBI if it resulted directly from enemy action, was medically documented, and involved loss of consciousness or altered mental status.
Also read: Central Sleep Apnea and Traumatic Brain Injury in Veterans Disability
At Prestige Veteran Medical Consulting, a veteran-owned company, we specialize in Independent Medical Opinions (IMOs) known as Nexus letters.
Our purpose is to empower YOU, the veteran, to take charge of your medical evidence and provide you with valuable educational tools and research to guide you on your journey.
Understanding the unique challenges veterans face, our commitment lies in delivering exceptional service and support.
Leveraging an extensive network of licensed independent medical professionals, all well-versed in the medical professional aspects of the VA claims process, we review the necessary medical evidence to incorporate in our reports related to your VA Disability Claim.
Prestige Veteran Medical Consulting is not a law firm, accredited claims agent, or affiliated with the Veterans Administration or Veterans Services Organizations. However, we are happy to discuss your case with your accredited VA legal professional.














One Response