Last Updated on 11 September, 2025
Irritable Bowel Syndrome (IBS) is a complex medical condition with symptoms that can significantly impact a person’s quality of life. Leah analyzes the relationship between irritable bowel syndrome and PTSD in veterans’ disability. She also explores how the VA rates these secondary connection claims and what evidence veterans can provide to secure the compensation and medical care they’ve earned through their service.

Table of Contents
What is Irritable Bowel Syndrome (IBS) in Veterans?
Irritable Bowel Syndrome (IBS) is a functional gastrointestinal disorder affecting the large intestine. Typically diagnosed using the Rome criteria, IBS is defined by a cluster of persistent gastrointestinal symptoms lasting six months or more that cannot be attributed to any other medical condition. It causes chronic, often debilitating symptoms such as abdominal pain, diarrhea, constipation, gas, bloating, and an urgent or incomplete need to defecate.
IBS is classified into three types:
- IBS-D (with diarrhea)
- IBS-C (with constipation)
- IBS-M (mixed type)
For veterans, IBS may develop due to multiple service-related factors, including:
- Chronic stress from combat exposure
- Military sexual trauma (MST)
- Traumatic brain injury (TBI)
- Poor field nutrition and sanitation
- Frequent use of antibiotics or NSAIDs
As per the VA Annual Benefits Report for FY2024, over 286,081 veterans are service-connected for IBS. Notably, Irritable Bowel Syndrome is especially common among Gulf War veterans for whom it is recognized as a presumptive condition under MUCMI (Medically Unexplained Chronic Multisymptom Illness).
Ultimately, IBS among veterans, more than a digestive issue, is often the physical manifestation of unresolved psychological trauma. When properly documented and service-connected, it qualifies for VA disability compensation, especially when claimed as secondary to mental health conditions like PTSD and anxiety.
VA Disability Ratings for IBS Secondary to PTSD
The VA rates Irritable Bowel Syndrome (IBS) under 38 CFR § 4.114 (Schedule of ratings—digestive system), Diagnostic Code 7319. The ratings for IBS secondary to PTSD are the same as for primary IBS, with compensation based on symptom severity, frequency, and impact on daily life.
30% VA Rating (Severe):
- Abdominal pain related to defecation at least once per week
- Plus 2 or more of the following:
- Change in stool frequency or form
- Urgency or straining
- Mucorrhea
- Bloating or distension
20% VA Rating (Moderate):
- Abdominal pain for at least three days per month
- Plus 2 or more of the above symptoms
10% VA Rating (Mild):
- Abdominal pain at least once in the past three months
- Plus 2 or more of the above symptoms
Update: As of May 2024, the VA eliminated the 0% non-compensable rating for IBS. All veterans with qualifying symptoms will receive at least a 10% rating.
89 FR 19735 (Mar. 20, 2024) (effective May 19, 2024).
This update ensures that even mild but chronic IBS symptoms now qualify for monthly compensation.
Veterans who experience regular GI symptoms should document flare-ups, treatment history, and limitations in daily life to receive an appropriate IBS secondary to PTSD rating.
PTSD: Root Cause of Many Secondary Disabilities
Post-Traumatic Stress Disorder (PTSD) is a mental health condition triggered by exposure to traumatic events such as combat, IED explosions, military sexual trauma (MST), deployment in hostile environments, or witnessing the death of fellow service members.
PTSD causes long-lasting physical and behavioral symptoms that can often interfere with daily life and may develop or aggravate secondary conditions like IBS, GERD, hypertension, and migraines.
Common PTSD symptoms include:
- Flashbacks, nightmares, and intrusive thoughts
- Avoidance of people or places
- Hypervigilance and irritability
- Depression, anxiety, and sleep disturbances
- Difficulty concentrating
- Panic attacks
These ongoing symptoms can strain the autonomic nervous system, which also regulates gut function, helping to explain the frequent co-occurrence of IBS and mental health disorders in veterans.
The Journal of Clinical Gastroenterology study “Prevalence of Gastrointestinal Symptoms and Disorders in Veterans with PTSD” found that 25% of veterans living with PTSD had symptoms that met the diagnostic criteria for IBS.
Women veterans are especially vulnerable, with nearly 38% reporting IBS symptoms in VA clinical settings, which were significantly more common among those with PTSD.
PTSD VA Disability Ratings
The VA rates PTSD using the General Rating Formula for Mental Disorders under 38 CFR § 4.130 (Schedule of ratings – Mental Disorders), Diagnostic Code 9411. Ratings for PTSD range between 0%, 10%, 30%, 50%, 70%, and 100% based on the severity and impact of the condition on occupational and social functioning.
|
Rating |
Impact / Key Symptoms |
|
100% |
Total occupational & social impairment; delusions, hallucinations, danger to self/others, disorientation, severe memory loss. |
|
70% |
Severe impairment; suicidal ideation, obsessional rituals, near-continuous panic/depression, neglect of hygiene, inability to maintain relationships. |
|
50% |
Reduced reliability/productivity; flattened affect, frequent panic, impaired judgment/thinking, motivation/mood disturbance, relationship difficulty. |
|
30% |
Occasional decrease in work efficiency; depressed mood, anxiety, weekly panic, sleep problems, mild memory loss. |
|
10% |
Mild/transient symptoms; decreased efficiency under stress or controlled by medication. |
|
0% |
Diagnosed, but no significant impairment or medication needed. |
A service-connected PTSD diagnosis is often the foundation for claiming secondary conditions like Irritable Bowel Syndrome.
How does PTSD lead to IBS? Key Mechanisms
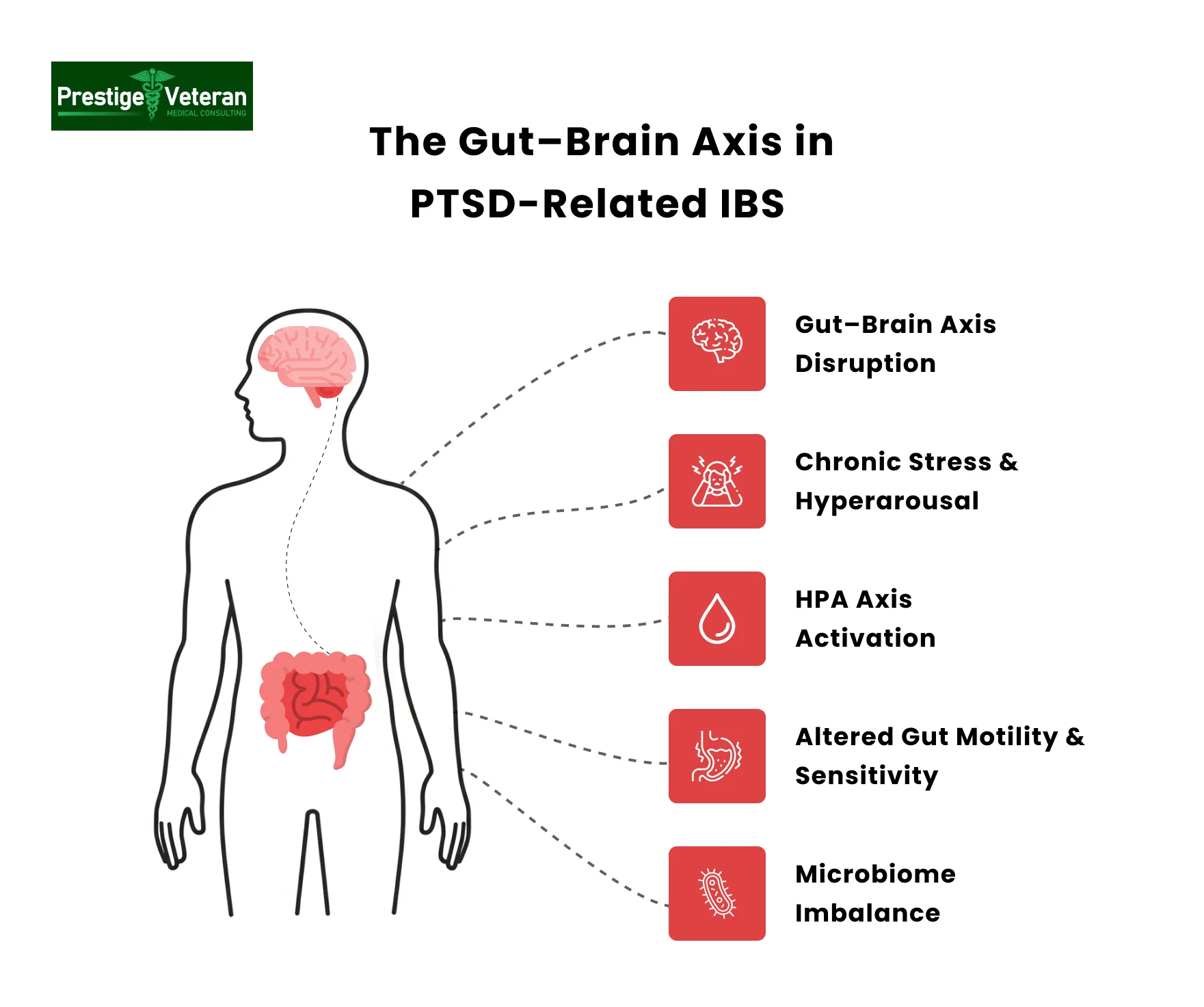
The connection between Post-Traumatic Stress Disorder and Irritable Bowel Syndrome is rooted in the complex, bidirectional relationship between mental health and gastrointestinal function. Below are the key biological and psychological mechanisms connecting PTSD to IBS in veterans:
- Gut–Brain Axis Disruption: PTSD disrupts the gut–brain axis, the essential communication link between the central nervous system and the gastrointestinal tract. This disruption leads to abnormal digestive function and heightened gut sensitivity, making veterans more prone to gastrointestinal distress.
- Chronic Stress and Hyperarousal: Veterans with PTSD often endure prolonged stress and hypervigilance. Often called the “second brain,” the gut reacts to chronic stress, where altered hormones and neurotransmitters disrupt normal bowel function and trigger digestive discomfort.
- HPA Axis Activation: Persistent activation of the hypothalamic–pituitary–adrenal (HPA) axis elevates stress hormones such as cortisol. These heightened cortisol levels impair gut motility, alter digestion speed, and increase visceral pain sensitivity, which are key features linked to IBS.
- Altered Gut Motility and Sensitivity: Due to these physiological changes, veterans may experience irregular bowel movements, abdominal cramping, bloating, diarrhea, or constipation, as the gastrointestinal tract becomes increasingly reactive to everyday stimuli.
- Microbiome Imbalance: PTSD-related stress disrupts the diversity and composition of gut bacteria, triggering inflammation and making veterans more susceptible to IBS symptoms.
- Veteran Populations at Higher Risk: Combat exposure and military sexual trauma intensify stress responses, leaving veterans with PTSD disproportionately vulnerable to post-traumatic IBS compared with the general population.
Recognizing this link underscores the need for integrated care. Treating PTSD holistically with mental health support, stress management, and GI-focused interventions can reduce IBS severity and improve overall quality of life for veterans.
Recognized Link Between PTSD and IBS
Research suggests a strong link between PTSD and gastrointestinal disorders, including IBS. One study published in the Journal of Neuroscience and Rural Practice in 2015 explores the connection, discussing the impact of the emotional limbic system, increased release of hormones, and cortisol on the enteric nervous system, leading to IBS symptoms. Other articles, such as “Post Traumatic Stress Disorder and Gastrointestinal Disorders in Danish Populations” and “Irritable Bowel Syndrome, Anxiety, and Depression: What are the Links?” provide further insights.
The study, “The relationship between post-traumatic stress disorder and gastrointestinal disease in United States Military Veterans,” reported that PTSD is bidirectionally associated with multiple gastrointestinal diseases, including IBS, suggesting that clinicians should screen for GI disease in trauma patients (and vice versa). It was also found that on average, veterans with PTSD are 2.73 times more likely to suffer from IBS compared with other veterans.
One meta-analysis reported that individuals with PTSD have nearly threefold higher odds of irritable bowel syndrome, indicating a strong association between PTSD and IBS prevalence.
Medical Literature Supporting Your Claim
When seeking service connection for IBS and PTSD, it’s essential to provide relevant articles to support your case. Some recommended articles include those published in the Journal of Neuroscience and Rural Practice (2015), Epidemiology (PTSD and Gastrointestinal Disorders), and the Journal of Clinical Psychiatry (IBS, Anxiety, and Depression). These articles can be presented to primary care managers, VA doctors, or during Compensation and Pension (C&P) exams.
How to Prove IBS for a VA Disability Claim
To receive VA disability for IBS, you must show that the condition is either directly service-connected or secondary to an already service-connected condition.
If diagnosed during active service and the symptoms persist, Irritable Bowel Syndrome can be directly connected to service. Gulf War veterans, former POWs, or those exposed to contaminated food/water during that period may also be eligible for direct service connection.
Additionally, IBS can be secondary to other service-connected conditions, particularly mental health disorders like PTSD.
To obtain a VA disability for irritable bowel syndrome secondary to PTSD, you must meet three key elements (see 38 C.F.R. § 3.310):
- Current diagnosis: You must have a confirmed IBS diagnosis in your medical records (VA or private).
- Service-Connected PTSD: Irritable Bowel Syndrome must be linked to an already service-connected PTSD claim.
- Medical Nexus Letter: The connection (nexus) between PTSD and IBS must be clearly established by a qualified healthcare provider.
Veterans should also provide lay statements and evidence of symptoms worsening during PTSD flare-ups. With proper documentation, you can significantly improve the chances of an approved secondary claim and increased overall disability compensation.
How to File a VA Claim for IBS Secondary to PTSD
Filing a VA disability claim for IBS secondary to PTSD requires careful documentation and adherence to the VA’s claims process. Follow these steps:
Step 1: Gather Required Evidence
- A diagnosis of IBS (preferably from a GI specialist)
- VA rating decision letter for an existing service-connected PTSD
- A nexus letter from a medical provider explaining how PTSD caused or aggravated IBS
- Medical records (VA and private)
- Lay statements, if available
Step 2: Complete VA Form 21-526EZ
Fill and complete VA Form 21-526EZ – Application for Disability Compensation and Related Compensation Benefits. Clearly indicate that IBS is “secondary to PTSD.” Attach all supporting evidence, including medical records, service treatment records, nexus letters, DBQs, and lay evidence.
Step 3: Submit Your Claim
- Online via VA.gov
- By mail to: Department of Veterans Affairs, Claims Intake Center, P.O. Box 4444, Janesville, WI 53547-4444
- In person at your local VA regional office
- With the assistance of a Veteran Service Organization (VSO) or VA-accredited attorney
Step 4: Attend the C&P Exam
After your claim is submitted, the VA may schedule a Compensation & Pension (C&P) exam to assess the severity of your symptoms and verify secondary service connection. Attend the exam, bring supporting documentation, and be ready to explain your symptoms to the examiner.
Step 5: Monitor and Appeal If Needed
Track your claim or appeal status and be prepared to appeal if denied. Many secondary claims are approved during supplemental reviews or BVA appeals.
Veterans may work with a VA-accredited Veterans Service Organization (VSO), such as DAV or VFW, or seek legal representation to ensure the strongest possible submission.
Is IBS a Presumptive Condition Under the PACT Act?
Irritable Bowel Syndrome is not currently included as a presumptive condition under the Honoring Our PACT Act of 2022, which expanded benefits for veterans exposed to toxic substances. However, the VA does recognize IBS as a presumptive condition for Gulf War veterans and former Prisoners of War (POWs) under 38 CFR § 3.317.
For these veterans, the VA presumes IBS is service-connected, meaning no nexus letter is required to prove its link to military service.
You may qualify for presumptive IBS benefits if:
- You served in the Persian Gulf War in Southwest Asia or nearby regions (including Afghanistan, Syria, Turkey, Egypt, Jordan, Israel)
- You have a diagnosis of IBS that began during service or within 10 years of discharge
- You were held as a POW for 30 days or more
- Your IBS is considered part of a Medically Unexplained Chronic Multisymptom Illness (MUCMI)
Though IBS is not listed under the PACT Act presumptives, veterans exposed to toxic substances may still pursue service connection with proper medical evidence. Veterans must still submit VA Form 21-526EZ and meet the diagnostic criteria for IBS to qualify.
Individual Unemployability for IBS and PTSD Claims
Veterans whose IBS and PTSD symptoms severely impair their ability to work may qualify for Total Disability based on Individual Unemployability (TDIU). TDIU pays at the 100% disability rate, even if your combined rating is less. Symptoms such as chronic diarrhea, frequent bathroom breaks, abdominal pain, and PTSD-related anxiety can prevent steady job performance.
To qualify under 38 CFR § 4.16(a), a veteran must have:
- One service-connected disability rated at 60% or more, OR
- Multiple service-connected disabilities with one rated at 40%, and a combined rating of 70% or more.
Veterans who do not meet the rating thresholds may still qualify for extraschedular TDIU under § 4.16(b) by proving they are unemployable due to service-connected conditions.
Applying for TDIU typically involves submitting VA Form 21-8940 and providing thorough evidence of unemployability. Documentation such as medical opinions, employment history, and lay statements from coworkers can help prove how IBS flare-ups interfere with work.
IBS C&P Exam: What to Expect
The Compensation & Pension (C&P) exam for IBS is the VA’s way of confirming the severity, frequency, and impact of your symptoms. Being honest, thorough, and prepared ensures the C&P examiner has the information needed for a fair decision.
During the exam, be ready to discuss:
- Symptom history: When Irritable Bowel Syndrome began, treatments tried, and any diagnostic tests (endoscopy, imaging, labs).
- Current symptoms: Abdominal pain, stool consistency, frequency and urgency of bowel movements, constipation or diarrhea, bloating, mucorrhea.
- Flare-ups: How often they occur, duration, triggers, and effects on work or daily activities.
- Documentation: Bring medical records, treatment notes, and your personal symptom diary or diet log.
If claiming IBS, the examiner will use the Intestinal Conditions Disability Benefits Questionnaire to rate the frequency of pain related to defecation, urgency, stool change, and other functional digestive symptoms. This standardized form allows examiners or private doctors to translate your symptoms into rating criteria, helping the VA assign an accurate disability percentage.
Secondary Conditions Related to IBS and PTSD
Veterans suffering from IBS and PTSD often experience other related conditions that may also be rated separately or claimed secondarily, including:
- GERD (Gastroesophageal Reflux Disease)
- Hemorrhoids (aggravated by IBS-related straining or diarrhea)
- Diverticulitis secondary to PTSD
- Generalized Anxiety Disorder
- Depression
- Fibromyalgia
- Chronic Fatigue Syndrome
- Migraines
- Medication-induced gastrointestinal issues (from NSAIDs used for pain)
If you’re suffering from multiple conditions, consider filing for secondary claims to increase your overall VA disability rating and receive treatment for the full scope of your health challenges.
Note: VA won’t rate the same symptoms twice to avoid “pyramiding”. For instance, if IBS, GERD or functional dyspepsia cause overlapping pain, diarrhea, or bloating, you may receive only one rating. Distinct, well-documented manifestations may justify separate ratings with evidence.
Tips for Proving IBS Secondary to PTSD for VA Disability
Below are five helpful strategies to establish a secondary service connection for IBS linked to PTSD.
1. Obtain a High-Probative Nexus Letter
A nexus letter from a qualified medical professional should clearly state that the veteran’s irritable bowel syndrome is “at least as likely as not” caused or aggravated by service-connected PTSD.
Ensure the nexus letter references:
- Your C-file details
- Medical literature on the gut-brain axis relationship between PTSD and IBS
- Physician’s credentials and rationale
- Review of military and treatment history
Medical opinions from physicians familiar with VA standards, especially gastroenterologists or mental-health providers, can add credibility.
2. Document Symptom Patterns in Detail
Veterans should keep a daily log of abdominal pain, diarrhea, constipation, and flare-ups triggered by PTSD symptoms. This helps show the VA how post-traumatic IBS disrupts work, relationships, and daily living, which is critical for a higher disability rating.
3. Explain the Gut-Brain Axis in Your Medical Evidence
When possible, submit peer-reviewed research showing that PTSD and IBS share the gut–brain axis connection. Including studies from VA medical centers or other credible medical literature can strengthen your argument for Board of Veterans’ Appeals decisions.
4. Highlight Secondary and Aggravated Conditions
If GERD, hemorrhoids, or diverticulitis secondary to PTSD or IBS exists, note them in the claim. These secondary conditions can increase the combined VA rating for IBS and related issues.
5. Prepare Thoroughly for the C&P Exam
At your Compensation & Pension (C&P) exam, explain the frequency, intensity, and duration of your IBS symptoms clearly.
Focus on your worst days, for instance, “When I experience severe stress, my IBS causes repeated cramping and urgent diarrhea multiple times a day, making it impossible to leave home or complete normal activities.”
Bring supporting evidence, including a written symptom diary, prescriptions, buddy statements, and proof of missed work or appointments due to IBS.
Illustrative Cases: VA Rating for IBS Secondary to PTSD
Case 1 – IBS Secondary to Combat-Related PTSD with GERD
A 37-year-old Iraq veteran developed persistent diarrhea, abdominal cramping, and bloating several years after deployment. Already service-connected for PTSD, he also reported chronic heartburn and regurgitation diagnosed as GERD.
His gastroenterologist issued a nexus letter linking chronic stress to both IBS and GERD, and he kept detailed logs showing three to six urgent bowel movements and frequent reflux episodes during PTSD flare-ups.
With this evidence and buddy statements from coworkers, the VA granted a combined 30% rating, 20% for secondary IBS, 50% for primary service-connected PTSD, plus 10% for GERD as a separate, distinct condition.
Case 2 – IBS Secondary to MST-Related PTSD
A 40-year-old Navy veteran experienced ongoing abdominal pain, alternating constipation and diarrhea, and bloating. She was service-connected for PTSD related to military sexual trauma and submitted VA and private treatment records showing worsening IBS during anxiety flare-ups.
She provided buddy statements and a food/symptom diary. A GI specialist supported the gut–brain link in a nexus letter. The VA awarded a 30% IBS rating secondary to PTSD due to frequent incapacitating episodes and disruption of daily activities.
Disclaimer: This article is general information and not meant for medical advice or legal advice. It is best to seek guidance on secondary claims from an expert legal professional like a Veterans Service Officer (VSO), accredited claims agent, or attorney.
Conclusion
Navigating the complexities of service connection for Irritable Bowel Syndrome and PTSD requires a thorough understanding of the conditions, their connections, and the VA’s rating system. Veterans are encouraged to gather relevant medical evidence, including articles supporting the link between PTSD and IBS. Seeking assistance from a VSO or legal professional is often important to ensure the best possible outcome in their disability claims. By advocating for their rights and presenting a well-documented case, veterans can improve their chances of receiving the compensation and care they deserve.
FAQs
Is IBS recognized as secondary to PTSD?
Yes, IBS can be rated as a secondary condition to service-connected PTSD due to the gut-brain axis disruption caused by chronic stress and trauma.
How do I prove IBS for a VA disability claim?
To prove IBS for VA disability, you need a current IBS diagnosis, service connection (direct or secondary), and a medical nexus linking it to your military service or PTSD.
What health issues are secondary to PTSD?
Common conditions secondary to PTSD include depression, anxiety, migraines, Irritable Bowel Syndrome, GERD, hypertension, and chronic fatigue syndrome.
Can you develop IBS from post-traumatic stress disorder?
Yes, PTSD can lead to the development of IBS through chronic stress, gut–brain axis disruption, hormonal changes, and microbiome imbalance.
What is the VA rating for IBS secondary to PTSD?
The VA rates IBS secondary to PTSD at 10%, 20%, or 30%, based on symptom severity, frequency, and impact on daily life.
How do I get a 30% VA disability rating for IBS?
To receive a 30% VA rating for IBS, you must show severe symptoms, including weekly abdominal pain and at least two other issues like urgency, stool changes, mucorrhea, or bloating.
Also read: Understanding the New IBS VA Rating Criteria
At Prestige Veteran Medical Consulting, a veteran-owned company, we specialize in Independent Medical Opinions (IMOs) known as Nexus letters.
Our purpose is to empower YOU, the veteran, to take charge of your medical evidence and provide you with valuable educational tools and research to guide you on your journey.
Understanding the unique challenges veterans face, our commitment lies in delivering exceptional service and support.
Leveraging an extensive network of licensed independent medical professionals, all well-versed in the medical professional aspects of the VA claims process, we review the necessary medical evidence to incorporate in our reports related to your VA Disability Claim.
Prestige Veteran Medical Consulting is not a law firm, accredited claims agent, or affiliated with the Veterans Administration or Veterans Services Organizations. However, we are happy to discuss your case with your accredited VA legal professional.