Last Updated on 9 September, 2025
Insomnia, often overlooked in its connection to service-related disabilities, holds a significant place in the landscape of veteran health. In this article, Leah Bucholz examines the complex interplay between insomnia and mental health, with a special focus on its association with tinnitus. She also explores how this relationship shapes Veterans Affairs (VA) disability claims, offering veterans insights into securing fair ratings and compensation for insomnia when it develops as a secondary condition to tinnitus.

What is Insomnia?
For the purpose of VA disability ratings, insomnia is categorized as a mental health condition. According to the Diagnostic and Statistical Manual of Mental Disorders (DSM-5), insomnia is defined as a sleep-wake disorder. The DSM-5 outlines criteria for diagnosing insomnia, including dissatisfaction with sleep quality, difficulty initiating or maintaining sleep, early morning awakenings, and the persistence of these symptoms for at least three months.
The impact of insomnia extends beyond the realm of sleep, causing clinically significant distress or impairment in various areas of life. Notably, the sleep disorder should occur at least three nights per week, persist despite adequate opportunities for sleep, and not be exclusively related to other sleep disorders or substance use.
Table of Contents
Insomnia and Service Connection
To receive a VA rating for insomnia, veterans can establish a service connection on both primary and secondary bases.
Direct Service Connection
If a veteran was diagnosed with insomnia during their service, especially with a well-documented history, there is a likelihood of obtaining service connection on a direct or primary basis. However, individual circumstances, such as gaps in care or specific discharge issues, may influence the process.
Secondary Service Connection
On a secondary basis, physical conditions, including an already service-connected disability such as tinnitus, can contribute to or aggravate insomnia. Exploring this connection requires an understanding of the research and medical opinions associated with the relationship between tinnitus, mental health, and insomnia.
To establish a secondary service connection, the VA requires proof of three components:
- A current diagnosis of insomnia – documented by a licensed provider, often supported by sleep studies (polysomnography)
- An existing service-connected condition – such as tinnitus, which the VA must already rate.
- A medical nexus – a link between the two, typically provided via a nexus letter from a qualified medical professional stating that the insomnia is “at least as likely as not” caused or worsened by the primary condition.
Veterans should ensure that all three elements are thoroughly documented in their VA disability claim for insomnia secondary to tinnitus.
Tinnitus: A Contributing Factor
Tinnitus is the VA’s most commonly claimed condition, affecting more than 3.2 million veterans, as reported inthe Annual Benefits Report for Fiscal Year 2024. Generally, it is characterized by the perception of sound (ringing, buzzing, hissing) without an external source.
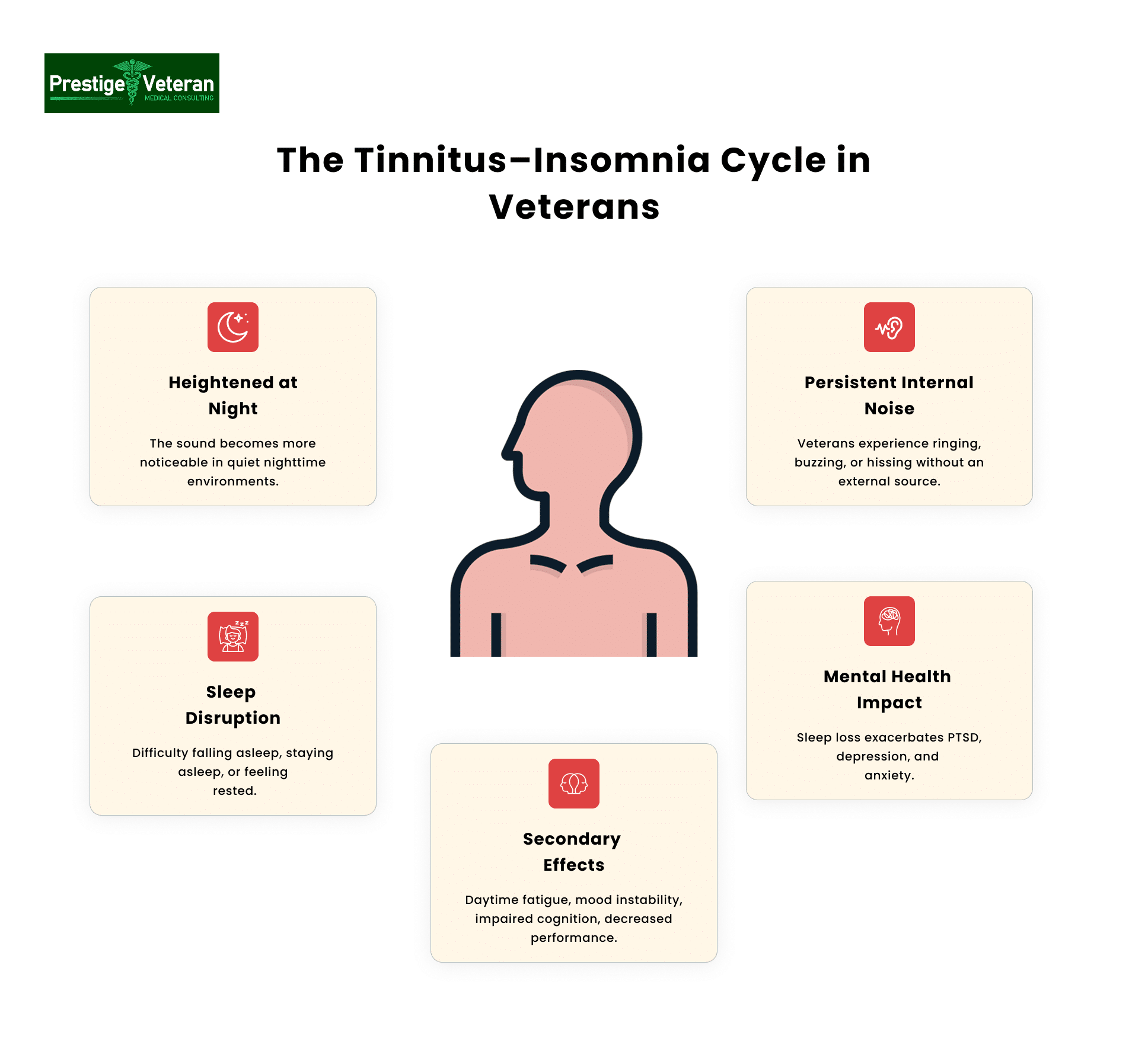
Veterans commonly report that the persistent internal noise becomes more noticeable in quiet nighttime settings, making it difficult to fall asleep, remain asleep, or experience restful sleep.
A 2015 cross-validation study found that 76% of patients with tinnitus also suffered from insomnia, underscoring the strong link between chronic tinnitus and sleep disturbances.
This ongoing sleep deprivation contributes to a range of secondary symptoms, including:
- Daytime fatigue
- Mood instability
- Impaired cognitive function
- Decreased work performance
Associations with Mental Health
Additionally, tinnitus-related sleep loss often exacerbates mental health ailments among veterans such as PTSD, depression, and anxiety, creating a complex clinical picture.
Studies, such as “Mental Health Symptoms Among Veterans VA Users by Tinnitus Severity,” highlight the predictive relationship between tinnitus severity and the intensity of other health issues. Tinnitus has been associated with mental health symptoms, emphasizing its connection to broader well-being.
Research articles like “Tinnitus and its Association with Mental Health and Health-Related Quality of Life in an Older Population” and “Correlation of the Tinnitus Handicap Inventory with Depressio,n Anxiety and Veterans with Tinnitus” delve into the nuanced relationship between tinnitus, mental health, and overall quality of life. These studies provide valuable insights for veterans seeking to establish a connection between their tinnitus and insomnia for VA disability claims.
This relationship is so well-established that tinnitus and insomnia are now frequently cited together in successful Board of Veterans’ Appeals (BVA) decisions.
Understanding VA Tinnitus Rating 2025
As of 2025, tinnitus continues to be rated under Diagnostic Code 6260 in the Schedule of ratings—ear (38 CFR § 4.87), with a maximum VA disability rating of 10%, regardless of whether it is unilateral or bilateral. Tinnitus is considered a subjective condition, meaning it relies heavily on the veteran’s self-reported symptoms.
Proposed Changes:
On February 15, 2022, the VA proposed to eliminate Diagnostic Code 6260 as a standalone rating for tinnitus. Under the proposal, tinnitus would no longer receive its own 10% rating but instead be evaluated only as part of an underlying condition. This rule has not yet been finalized, so DC 6260 and the single 10% rating remain in effect until further notice (Federal Register 87 FR 8474; VA-2022-VBA-0009).
VA Rating for Insomnia Secondary to Tinnitus
Understanding the VA disability ratings for insomnia is crucial for veterans navigating the claims process. Consulting legal professionals for accurate and up-to-date information is the best option, but a brief overview can shed light on the potential ratings:
The VA rates insomnia secondary to tinnitus under the General Rating Formula for Mental Disorders (38 CFR § 4.130). Because insomnia lacks its own diagnostic code, it is rated analogously to mental health conditions like anxiety or depression. Insomnia ratings range between 0%, 10%, 30%, 50%, 70%, and 100%, based on occupational and social impairment.
Here’s how insomnia VA disability ratings generally apply:
- 0% Rating: Diagnosed, but symptoms not severe enough to interfere in occupational or social settings.
- 10% Rating: Occupational or social impairment due to mild or transient symptoms.
- 30% Rating: Occupational and social impairment with decreased work efficiency and intermittent periods of inability to perform tasks.
- 50% Rating: Occupational and social impairment with reduced reliability.
- 70% Rating: Deficiency in most areas with occupational and social impairment.
- 100% Rating: Total occupational and social impairment.
These ratings reflect the severity of symptoms and their impact on daily functioning. Veterans should seek guidance from legal professionals to navigate the intricacies of the rating system.
Related Secondary Conditions to Insomnia and Tinnitus
Veterans filing for VA disability ratings for insomnia secondary to tinnitus should also be aware of the broader impact these conditions can trigger. Chronic sleep deprivation from tinnitus often sets off a cascade of secondary conditions that may increase overall ratings and strengthen claims.
Mental Health Conditions
Commonly linked are depression and anxiety, both recognized by the VA as ratable mental health conditions under 38 CFR § 4.130. Veterans frequently report irritability, intrusive thoughts, and heightened stress, all aggravated by poor sleep and constant ringing. Post-Traumatic Stress Disorder (PTSD) may also worsen with tinnitus-related insomnia, since hyperarousal and nighttime vigilance disrupt recovery and rest cycles.
Physical Health Conditions
On the physical side, prolonged insomnia contributes to hypertension, migraines, Meniere’s disease, and cardiovascular issues, conditions increasingly documented in medical literature as linked to chronic sleep disturbance.
Cognitive and Functional Impairments
Veterans may also experience cognitive impairments, including memory lapses, reduced concentration, and poor decision-making, which can support higher ratings for occupational and social impairment.
Documenting these secondary effects alongside insomnia with medical records, nexus letters, and lay statements can demonstrate the full scope of disability. By showing how tinnitus-induced sleep loss leads to related health problems, veterans position themselves for stronger VA claims, higher combined ratings, and potential eligibility for TDIU.
100% TDIU Compensation for Insomnia
Veterans whose tinnitus-related insomnia prevents them from working may be eligible for Total Disability based on Individual Unemployability (TDIU). This provides compensation at the 100% disability rate, even if the veteran’s combined rating is below 100%.
To be eligible for schedular TDIU (38 C.F.R. § 4.16(a)), a veteran must have:
- One condition must be rated at 60%, or
- Multiple conditions with a combined rating of 70%, including one rated at 40%.
For example, a veteran rated at 10% for tinnitus, 30% for insomnia, and 50% for depression may meet the TDIU schedular threshold (a combined rating of 70%) if unable to work due to symptoms like fatigue, memory issues, or concentration problems.
If a veteran does not meet these rating thresholds, extraschedular TDIU (38 C.F.R. § 4.16(b)) may still be granted. The VA considers the veteran’s unique circumstances, supported by employer statements, medical opinions, SSA records, or vocational assessments. Veterans should include this request in their initial claim or file it separately using VA Form 21-8940.
How to File a VA Claim for Insomnia Secondary to Tinnitus
For veterans suffering from chronic sleep deprivation due to tinnitus, here is a detailed breakdown of how to successfully file your claim.
1. Confirm Tinnitus is Service-Connected
To claim insomnia as a secondary condition, you must already have an approved VA rating for tinnitus, typically rated at 10%.
2. Get a Confirmed Diagnosis of Insomnia
Obtain a formal diagnosis of insomnia from a VA or private provider. Sleep studies, psychiatric evaluations, and treatment history may strengthen your VA insomnia claim.
3. Obtain a Nexus Letter Linking Insomnia to Tinnitus
A nexus letter for insomnia secondary to tinnitus must come from a qualified medical professional (e.g., psychologist, psychiatrist, sleep specialist) and clearly state that your insomnia is “at least as likely as not” caused or aggravated by tinnitus. It should cite medical literature and explain the pathophysiology.
4. Gather Supporting Evidence Demonstrating Functional Impairment
To receive a favorable VA rating for insomnia secondary to tinnitus, you must show how your sleep disorder affects your work performance, relationships, and daily life.
Include evidence in your VA claim, like:
- Sleep studies
- VA or civilian medical records
- Buddy statements from spouses, friends, or coworkers describing the impact on daily functioning
- Personal statements
- Sleep journal
5. File VA Form 21-526EZ
Use VA Form 21-526EZ to submit your claim online, by mail, or in-person at a VA Regional Office. Clearly list “insomnia secondary to tinnitus” and attach your nexus letter and supporting documents.
6. Prepare for a C&P Exam
Expect to attend a Compensation & Pension (C&P) exam, where a VA examiner will evaluate both the severity of your insomnia and its relationship to your tinnitus. Describe how sleep deprivation affects your mood, work, and daily activities.
7. Track Your Claim and Respond to the VA
After filing, monitor your claim status via VA.gov or call 1-800-827-1000. Be prepared to respond to any Requests for Evidence (RFEs) quickly. If your secondary service connection is denied, consider filing a supplemental claim, requesting a Higher-Level Review, or directly appealing to the Board of Veterans’ Appeals.
You can consult a VA-accredited claims agent, Veterans Service Organizations (VSOs), or attorneys to ensure your submission is complete with documentation.
Nexus Letter: The Missing Link in Your Tinnitus-Insomnia Claim
A nexus letter is crucial in establishing insomnia as a secondary condition resulting from primary service-connected tinnitus.
To be effective, the medical nexus letter should:
- Be authored by a credentialed physician
- Use VA-accepted terminology like “at least as likely as not”
- Explain the pathophysiological link between tinnitus and sleep disruption
- Reference relevant scientific literature
- Support the opinion with objective medical evidence, e.g. documented sleep disturbances, sleep study results, veteran’s service history
An independent medical opinion from a qualified professional bolsters your claim by providing expert, evidence-based linkage between the conditions. This “evidentiary bridge” demonstrates to the VA adjudicator that insomnia isn’t standalone but a direct consequence of tinnitus, significantly improving your chances of an approval or favorable rating.
Veterans can obtain nexus letters through independent medical examiners (IMEs), many of whom are former VA examiners or service members themselves.
When it comes to proving secondary conditions, a nexus letter may strengthen VA disability claims and counter low or denied initial ratings.
Case Study: Sleep Disturbance Due to Persistent Tinnitus
The Veteran served on active duty in the U.S. Army from September 1975 to September 1978. He sought service connection for insomnia, originally filed as “sleep disturbances,” asserting that persistent service-connected tinnitus caused his inability to fall and remain asleep.
Medical evidence confirmed a current diagnosis of insomnia. A March 2017 VA examiner noted chronic sleep impairment but opined it was unrelated to tinnitus, focusing instead on depression and hearing loss. However, multiple providers, including a VA psychologist and a private physician, directly linked the Veteran’s tinnitus to his ongoing sleep impairment, emphasizing the role of constant ringing in his ears.
The Board weighed this conflicting evidence alongside the Veteran’s credible lay statements. Applying the principle of reasonable doubt, the Board determined that his insomnia was at least as likely as not caused by tinnitus. Consequently, service connection for insomnia, secondary to tinnitus, was granted.
Source: Citation Nr: A20015990, Board of Veterans’ Appeals, Oct 26, 2020.
Common Mistakes to Avoid in an Insomnia Secondary to Tinnitus VA Claim
Veterans pursuing a VA rating for insomnia secondary to tinnitus often face specific challenges that can delay or derail their claim. Here are some key mistakes to avoid and strengthen your insomnia VA claim.
1. Failing to Establish Service Connection for Tinnitus First
Before claiming insomnia secondary to tinnitus, veterans must have tinnitus already recognized as service-connected. Without this foundational primary condition rating, the VA cannot legally consider a secondary link.
2. Not Providing a Strong Nexus Letter
One of the most common reasons the VA denies a claim is submitting a weak or no nexus letter for insomnia secondary to tinnitus. This letter must:
- Clearly state that the insomnia is “at least as likely as not” related
- Include medical reasoning
- Give citations to relevant research (such as studies showing 76% of tinnitus sufferers also experience insomnia
- Mention the physician’s credentials
Without this expert medical justification, the VA may not assume a secondary service connection.
3. Underreporting Symptoms During C&P Exams
During the VA Compensation & Pension (C&P) exam, minimizing how tinnitus and insomnia affect your daily life can lead to a lower rating. Since a chronic insomnia VA rating depends on the level of occupational and social impairment, avoid saying things like “I’m fine” or “it’s not that bad.” “Instead, give statements like, “The lack of sleep makes me irritable and short-tempered, which is straining my relationship with my family.”
4. Missing or Weak Medical Evidence
Many veterans lose out on disability benefits due to insufficient documentation. Veterans must present a current diagnosis of insomnia and its nexus to tinnitus, sleep studies, treatment records, and mental health notes showing consistent, chronic impact on daily life and functioning. Without this, the VA may view insomnia as unrelated or attribute it to other causes like aging or stress.
5. Misunderstanding VA’s Rating Criteria for Insomnia
Many veterans believe insomnia will be rated separately, but the VA rating for insomnia secondary to tinnitus is assigned under the General Rating Formula for Mental Disorders. That means your symptoms must align with VA’s mental health rating percentages: 0%, 10%, 30%, 50%, 70%, or 100%. Veterans must demonstrate functional impairments such as memory loss, panic attacks, or the inability to maintain employment.
6. Not Documenting Symptoms and Functional Impact
The VA heavily assigns disability ratings based on how insomnia affects occupational and social functioning. Many claims often fall short because veterans don’t maintain detailed logs of sleep loss, daytime fatigue, or work impairment. Hence, a well-kept sleep journal can strengthen an insomnia VA claim.
7. Filing Insomnia as a Standalone Claim
Do not file insomnia as an independent condition unless you can prove a direct service connection. Submitting it as a standalone condition without linking it to a primary service-connected disability, such as tinnitus, will likely result in the VA denying your claim.
8. Overlooking Related Secondary Conditions
Tinnitus-related sleep deprivation often leads to depression, anxiety, or even PTSD exacerbation. Veterans who experience these symptoms may be eligible for higher combined ratings. For instance, a veteran with tinnitus, insomnia, and depression might qualify for TDIU (Total Disability based on Individual Unemployability) if they cannot maintain gainful employment.
By avoiding these pitfalls, veterans can significantly improve their chances of securing a favorable VA disability claim for insomnia linked to tinnitus.
Disclaimer: This article is for informational purposes only and is not medical or legal advice. Veterans should consult a licensed clinician for diagnosis/treatment and a VA-accredited representative or attorney for claims/appeals.
Navigating the VA Disability Landscape
Insomnia, often linked with mental health conditions, is a critical factor in the realm of VA disability claims. Leah Bucholz’s insights into the primary and secondary connections of insomnia, particularly with tinnitus, provide veterans with a roadmap for establishing service connection. Armed with an understanding of the DSM-5 criteria for insomnia, the relationship between tinnitus and mental health, and the VA disability ratings, veterans can approach the claims process with informed confidence. However, the complexity of the system necessitates collaboration with legal professionals to ensure a thorough and effective approach to VA disability claims.
FAQs
Can insomnia be linked to tinnitus?
Yes, tinnitus or constant ringing in the ears often disrupts sleep and is a well-established secondary cause of insomnia in veterans.
What are the top secondary conditions to tinnitus?
The top secondary conditions to tinnitus include insomnia, depression, anxiety, PTSD, migraines, and Meniere’s disease.
How can I claim anxiety secondary to tinnitus?
To claim anxiety secondary to tinnitus, you need a medical diagnosis, a nexus letter linking the two, and supporting evidence of functional impairment.
What mental issues can tinnitus cause?
Tinnitus can contribute to anxiety, depression, irritability, and other mood or cognitive disorders.
What is the average VA rating for insomnia?
The VA rating for insomnia varies widely from 0% to 100%, depending on occupational and social impairment, with many veterans receiving around 30%.
What is the VA rating for insomnia secondary to tinnitus?
Insomnia secondary to tinnitus is rated under the General Rating Formula for Mental Disorders, ranging between 0%, 10%, 30%, 50%, 70%, and 100% based on occupational and social impairment.
How can I obtain a 50% insomnia VA disability rating?
You can receive a 50% VA rating for insomnia if your symptoms cause reduced reliability and productivity in work or social functioning.
What sleep disturbances are secondary to tinnitus?
Tinnitus can cause difficulty falling or staying asleep, early awakenings, and non-restorative sleep, leading to chronic insomnia.
Also read: 9 Reasons VA Tinnitus Claims Are Denied: Tips to Support Your Appeals
At Prestige Veteran Medical Consulting, a veteran-owned company, we specialize in Independent Medical Opinions (IMOs) known as Nexus letters.
Our purpose is to empower YOU, the veteran, to take charge of your medical evidence and provide you with valuable educational tools and research to guide you on your journey.
Understanding the unique challenges veterans face, our commitment lies in delivering exceptional service and support.
Leveraging an extensive network of licensed independent medical professionals, all well-versed in the medical professional aspects of the VA claims process, we review the necessary medical evidence to incorporate in our reports related to your VA Disability Claim.
Prestige Veteran Medical Consulting is not a law firm, accredited claims agent, or affiliated with the Veterans Administration or Veterans Services Organizations. However, we are happy to discuss your case with your accredited VA legal professional.















