Last Updated on 8 September, 2025
Hypertension, commonly known as high blood pressure, is a prevalent health concern, especially among veterans, and it often goes hand in hand with mental health challenges like Post-Traumatic Stress Disorder (PTSD). In this blog, Leah Bucholz sheds light on the relationship between hypertension and PTSD in veterans’ disability.
The Department of Veterans Affairs (VA) recognizes hypertension as a condition that may be service-connected, either directly or as secondary to PTSD. Understanding this link is critical for veterans seeking disability benefits, as it highlights both the physical and psychological toll of military service.

Table of Contents
Defining Hypertension
Hypertension occurs when the pressure of circulating blood against the blood vessels is consistently higher than the norm, as defined by medical professionals. The World Health Organization classifies high blood pressure based on systolic pressure (when the heart beats) and diastolic pressure (when the heart rests between beats). A systolic pressure exceeding 140 or a diastolic pressure over 90 is considered hypertension.
The American College of Cardiology and American Heart Association (2017) has defined “elevated blood pressure” as systolic readings between 120 and 129 with diastolic below 80.
- Stage 1 hypertension is defined as systolic pressure between 130 and 139 mmHg or diastolic pressure between 80 and 89 mmHg.
- Stage 2 hypertension is defined as blood pressure of 140/90 mmHg or higher.
For VA disability purposes, hypertension must be confirmed by readings taken two or more times on at least three different days.
Prolonged, uncontrolled high blood pressure can damage arteries and organs, leading to:
- Heart disease
- Stroke
- Chronic kidney disease
- Vision loss
- Aneurysms
- Cognitive decline
In the VA Annual Benefits Report, around 750,278 veterans received disability compensation for hypertensive vascular disease in fiscal year 2024.
PTSD: A Common Service-Connected Condition
Post-Traumatic Stress Disorder (PTSD) is a psychiatric condition that can develop after experiencing or witnessing a traumatic event, common among veterans exposed to combat, military sexual trauma, or life-threatening situations during service. PTSD is one of the most common VA service-connected mental health disabilities, with over 1.5 million veterans receiving compensation as of recent data.
Symptoms of PTSD may include:
- Flashbacks, intrusive memories, or nightmares
- Avoidance of trauma reminders
- Severe anxiety or depression
- Hypervigilance and exaggerated startle response
- Irritability or anger
- Insomnia or chronic sleep problems
PTSD can severely impair a veteran’s ability to maintain relationships, employment, and daily functioning. Depending on the severity, it can lead to secondary health issues, such as hypertension, sleep apnea, GERD, or migraines.
VA statistics related to post-traumatic stress disorder show that:
- 11-20% of Iraq and Afghanistan veterans have PTSD in any given year
- 12% of Gulf War veterans have PTSD
- Up to 30% of Vietnam veterans have suffered from PTSD in their lifetime
The emotional toll of PTSD often translates into physical conditions, making a secondary claim to PTSD critical for many veterans. The VA recognizes medical conditions secondary to PTSD, including high blood pressure, allowing affected veterans to pursue additional compensation and benefits.
Can PTSD Cause Hypertension?
Yes, PTSD can cause or aggravate hypertension.
Scientific research supports the link between PTSD and hypertension. A large cohort study of over 200,000 U.S. veterans who served between 2001 and 2009 found that those with untreated posttraumatic stress disorder (PTSD) had a 24–46% higher risk of developing hypertension. Another 2018 study by the American Heart Association involving 3,846 U.S. service members from the Iraq and Afghanistan wars found that combat-injured soldiers with PTSD faced up to an 85% higher risk.
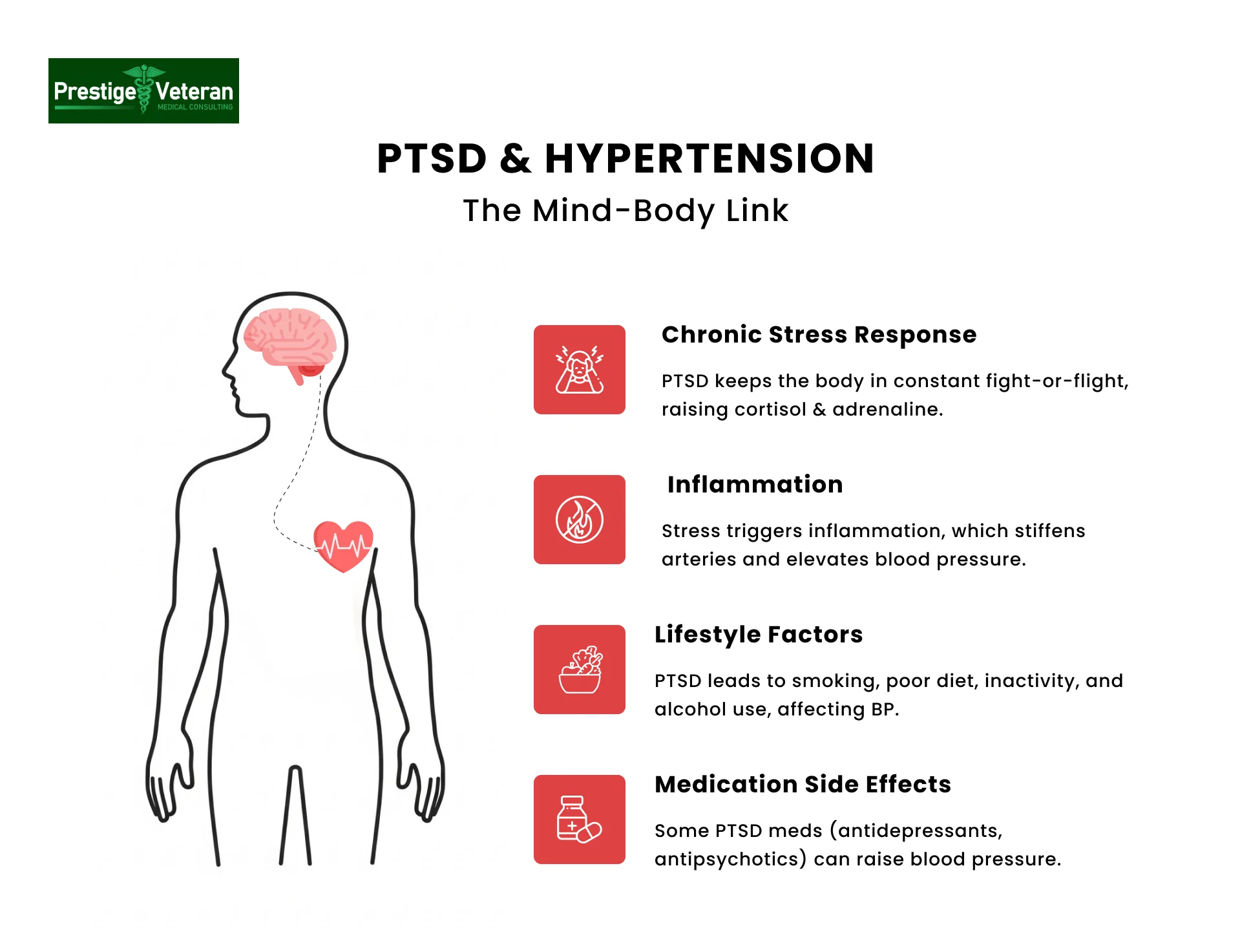
Here’s how PTSD affects blood pressure:
- Chronic Stress Response: PTSD keeps the body in a constant “fight or flight” mode, triggering stress hormones like cortisol and adrenaline, which can raise blood pressure.
- Inflammation: Ongoing stress increases inflammation throughout the body, stiffening arteries and contributing to high blood pressure.
- Lifestyle Factors: Veterans with hypertension are influenced by both non-modifiable factors, such as age and genetics, and modifiable factors related to PTSD, including weight, smoking, diet, activity, alcohol use, and stress. Obesity, when tied to service-connected conditions like PTSD or depression, can worsen hypertension.
- Medication Side Effects: Some drugs used to treat PTSD, including antidepressants and antipsychotics, may also elevate blood pressure.
Hypertension secondary to PTSD is a medically recognized condition, and veterans suffering from both are eligible to file for VA disability benefits.
Exploring the Link Between Hypertension and Mental Health
Mental health conditions, particularly PTSD, can contribute significantly to hypertension. There are several studies linking anxiety disorders to increased blood pressure. One such study, titled “Anxiety Disorders, Hypertension, and Cardiovascular Risk: A Review” (International Journal of Psychiatry and Medicine, 2011), highlights the role of psychological stress in raising autonomic arousal, leading to higher blood pressure.
The Impact of PTSD on Blood Pressure
Research studies like “Hypertension in Relation to Post-Traumatic Stress Disorder and Depression in the U.S. National Co-morbidity Survey” (Behavioral Medicine) and “The Impact of Post-Traumatic Stress Disorder on Blood Pressure and Heart Rate in a Veteran Population” (Journal of Traumatic Stress), delves into the relationship between PTSD, depression, and high blood pressure among veterans.
Understanding these scientific studies and surveys is vital for establishing a secondary service connection for PTSD and hypertension.
Secondary Service Connection for Hypertension
Veterans can be service-connected for high blood pressure through various avenues. If diagnosed while on active duty, individuals may establish a direct service connection. However, a single high reading does not necessarily suffice; a conclusive diagnosis typically requires a series of controlled readings over several days. This cautious approach aims to rule out external factors that may influence blood pressure, such as illness or equipment malfunctions.
How to Prove Secondary Service Connection
Another route to service connection involves hypertension as a secondary condition related to other health issues. Often, another service-connected disability may cause or aggravate hypertension. One such example is the intricate relationship between hypertension and mental health, particularly PTSD in many veterans.
Claiming Hypertension Secondary to PTSD
To receive compensation for high blood pressure secondary to PTSD, veterans must establish a secondary service connection, as outlined in 38 CFR § 3.310.
To prove a secondary claim for PTSD-related hypertension, three components are required:
- A current diagnosis of hypertension, confirmed by blood pressure readings on three different days
- Proof of a primary service-connected disability, such as PTSD
- A nexus letter from a medical provider stating that the veteran’s hypertension is “at least as likely as not” caused or aggravated by PTSD
A strong nexus letter written by a qualified healthcare professional should include a medical rationale, cite peer-reviewed literature, and explain the physiological link between PTSD and cardiovascular changes.
Once the secondary service connection is approved, the veteran will receive a separate VA disability rating for hypertension, which can increase their total combined rating and monthly compensation.
How the VA Rates Hypertension and PTSD
Leah Bucholz briefly touches on the ratings associated with hypertension service connection. These ratings are subject to change, and veterans are advised to consult professionals like Veteran Service Officers, accredited claims agents, and attorneys for the most accurate information.
VA Rating for Hypertension
The VA rates hypertension under Diagnostic Code 7101 (38 CFR § 4.104 – cardiovascular system) based on the severity of blood pressure readings:
- 10% Rating: Diastolic pressure predominantly 100 or more, or systolic pressure predominantly 160 or more, or minimum evaluation for an individual with a history of diastolic pressure predominantly 100 or more who requires continuous medication for control
- 20% Rating: Diastolic pressure predominantly 110 or more; systolic pressure predominantly 200 or more
- 40% Rating: Diastolic pressure predominantly 120 or more
- 60% Rating: Diastolic pressure predominantly 130 or more
To qualify for a VA disability claim, blood pressure must be recorded two or more times on at least three different days. Veterans on medication may still qualify based on historical readings or continuous treatment.
Leah emphasizes that even if medications control blood pressure within a normal range, veterans can still be service-connected.
PTSD VA Rating Criteria
Post-traumatic stress disorder is rated under 38 CFR § 4.130 using the General Rating Formula for Mental Disorders. VA ratings for PTSD are typically based on the severity of symptoms and their impact on occupational and social impairment:
- 0% Rating – PTSD diagnosed, but symptoms don’t interfere with work or social life
- 10% Rating – Mild or transient symptoms causing social and occupational impairment only during high stress, symptoms controlled with medication
- 30% Rating – Occasional work and social difficulty; issues like anxiety, depression, sleep disturbance, or mild memory loss, though daily functioning remains stable
- 50% Rating: Reduced reliability and productivity, frequent panic attacks, impaired judgment, memory or concentration problems, and difficulty maintaining social relationships
- 70% Rating: Serious impairment in most areas (work, school, family, judgment, mood); symptoms may include suicidal ideation, near-continuous depression or panic, poor impulse control, or inability to maintain relationships.
- 100% Rating: Total occupational and social impairment, often with hallucinations, grossly inappropriate behavior, danger to self/others, disorientation, memory loss, or inability to function independently
The VA evaluates both the severity of your symptoms and the functional impact when assigning a rating. Veterans often receive higher VA ratings when PTSD interferes significantly with work, family, or daily living. These ratings can be combined with a hypertension secondary to PTSD rating to increase total VA benefits.
TDIU – Total Disability Based on Individual Unemployability
Total Disability based on Individual Unemployability (TDIU) is a VA benefit for veterans who cannot maintain substantially gainful employment due to their service-connected conditions, even if they don’t have a 100% combined rating.
Hypertension and PTSD, when combined, can significantly impact concentration, energy levels, and emotional stability, which are barriers to gainful employment.
To qualify for schedular TDIU under 38 CFR § 4.16(a), a veteran must have:
- One condition rated at 60%, or
- Two or more conditions, with one at least 40% and a combined rating of 70% or more
For example, a veteran rated 50% for PTSD and 30% for hypertension meets the 70% threshold for schedular TDIU consideration. (See VA combined ratings table)
Even if these criteria aren’t met, extraschedular TDIU under § 4.16(b) may still apply if disabilities clearly prevent employment.
Veterans approved for TDIU receive compensation at the 100% disability rate, including access to expanded benefits such as CHAMPVA, Commissary privileges, and Dependents Educational Assistance (DEA).
To strengthen your TDIU claim, consider gathering opinions from a vocational expert or medical expert.
Filing Your VA Claim for Hypertension Secondary to PTSD
When filing a VA claim for hypertension as secondary to PTSD, it’s important to understand the process, gather the right evidence, and present a strong case to increase your chances of approval. Here’s a step-by-step process:
Step 1: Gather Evidence
- Current diagnosis of hypertension from a licensed medical provider
- Consistent blood pressure readings (2-3 times for over 3 separate days)
- Documentation showing service-connected PTSD, such as VA rating decisions or medical records
- Treatment history, e.g. prescribed medications, ongoing therapy, and blood pressure monitoring results
- Service treatment records (STRs)
- Private and VA medical records
Step 2: Obtain a Nexus Letter
Ask a qualified physician or a specialist, like a cardiologist or psychologist, to write a medical nexus letter explaining that your hypertension is “at least as likely as not” related to your PTSD. The provider should clearly explain their medical reasoning, citing clinical studies or known links between chronic stress and hypertension.
For example, your nexus letter doctor may cite studies linking chronic stress responses in PTSD to elevated blood pressure.
Step 3: Complete VA Form 21-526EZ
Once evidence is ready, complete and submit VA Form 21-526EZ (Application for Disability Compensation) to officially file your claim. Be sure to select “secondary condition” and attach all supporting documents like medical records, blood pressure logs, and the nexus letter with your submission.
Step 4: Submit the VA Claim
You can file online at VA.gov, by mail, or in person at your local VA Regional Office.
Step 5: Attend C&P Exam
After submission, the VA will likely schedule a Compensation & Pension (C&P) exam. Bring medication lists and be prepared to discuss how both PTSD and hypertension symptoms impact your daily life.
Step 6: Await VA Decision
If your claim is denied, consider appealing with a Higher-Level Review, a Supplemental Claim, or a Board Appeal.
Partnering with a Veterans Service Organization (VSO) or VA-accredited attorney can help ensure accurate documentation and strengthen your case for disability compensation.
How to Strengthen Your Claim for PTSD-Related Secondary Hypertension
When filing a VA disability claim, proving hypertension as secondary to PTSD requires more than medical records alone. Veterans must provide strong evidence, consistent documentation, and professional nexus opinions to build a well-supported claim.
Submit an Independent Medical Opinion (IMO)
A detailed Independent Medical Opinion strengthens your VA disability claim by providing a professional, unbiased nexus letter for hypertension secondary to PTSD. Ensure the nexus letter for hypertension secondary to PTSD should be written by a qualified healthcare provider and use VA language like “at least as likely as not” to link your high blood pressure to service-connected PTSD.
The provider should explain their medical reasoning and, ideally, reference peer-reviewed studies or VA/NIH research showing the connection between chronic stress responses in PTSD and high blood pressure.
Keep a Symptom Diary
Maintaining a daily journal documenting PTSD triggers, emotional stress, and blood pressure readings helps demonstrate a pattern. This real-world evidence reinforces that your high blood pressure is secondary to your psychological condition and supports your VA disability claim effectively.
Track Blood Pressure Readings Over Time
Use a reliable home blood pressure monitor and keep a log of your readings, especially if you experience fluctuations during periods of PTSD symptom flare-ups. This personal tracking should reflect VA’s requirement of consistent readings over time to confirm a hypertension diagnosis per Diagnostic Code 7101.
Provide Lay Statements (Buddy Letters)
Statements from family, friends, or coworkers who have witnessed the impact of your PTSD and how it may have worsened your physical health can support your claim.
For example, a spouse might write: “During panic episodes, his face reddens, blood pressure spikes, and he complains of pounding headaches,” showing hypertension linked to PTSD behaviors.
These statements are especially helpful when medical records are limited.
Maintain Consistent Treatment and Medication Records
Showing regular appointments and use of prescribed medications for both PTSD and hypertension can prove to the VA that your conditions are chronic and actively managed. It also demonstrates you are responsibly managing your health while reinforcing that your high blood pressure is directly linked to PTSD symptoms.
Demonstrate the Impact on Daily Life and Work
If hypertension and PTSD significantly impair your ability to work, consider filing for TDIU (Total Disability based on Individual Unemployability). Through combined ratings for PTSD and hypertension, veterans can meet the criteria for receiving 100% compensation.
Link Other Secondary Conditions
If you have any related conditions, such as high cholesterol, sleep apnea, or diabetes that exacerbate hypertension caused by PTSD, consider filing a secondary claim. Highlighting these comorbidities shows physiological deterioration from chronic psychological stress, strengthening the medical rationale of your claim and increasing chances of receiving higher VA disability compensation.
Case Study: Army Veteran with Hypertension Linked to PTSD
A 52-year-old Army veteran served two combat tours in Iraq. After service, he developed chronic PTSD with flashbacks, nightmares, and hypervigilance, rated at 50%. Over the next decade, he was diagnosed with stage 1 hypertension, averaging 140/90 mmHg, despite maintaining a healthy weight, diet, and regular exercise. Episodes of sharply elevated blood pressure were recorded during panic attacks and VA mental health sessions.
Initially, the VA denied his claim due to “insufficient evidence.” He later submitted the following evidence:
- An independent medical nexus opinion from a cardiologist citing PTSD-driven autonomic dysregulation as the aggravating factor
- VA treatment records showing BP spikes during PTSD episodes
- Blood pressure logs over multiple years
- Peer-reviewed studies establishing PTSD as a risk factor for cardiovascular disease
On reconsideration, the VA granted secondary service connection at a 10% rating.
This case highlights how proper medical documentation can shift a VA disability claim from denial to approval.
Sample Nexus Letter for Hypertension Secondary to PTSD
Subject: [Veteran’s Name – Redacted]
Date of Birth: [MM/DD/YYYY]
VA File Number: [Redacted]
Date: [Insert Current Date]
To Whom It May Concern,
I am [Dr. Full Name], a board-certified cardiologist, and I have thoroughly reviewed the medical history, treatment records, and service-related documentation for the above-named veteran. I am providing this independent medical opinion regarding the veteran’s diagnosis of hypertension and its relationship to his service-connected Post-Traumatic Stress Disorder (PTSD).
The veteran, a 44-year-old Marine Corps veteran deployed to Afghanistan in 2009, carries a well-documented diagnosis of chronic PTSD characterized by intrusive recollections, hypervigilance, panic episodes, and severe sleep disruption. Over time, his blood pressure readings have consistently met criteria for Stage 2 hypertension, with an average of 150/95 mmHg, despite adherence to prescribed antihypertensive therapy. Importantly, his clinical history is devoid of traditional risk factors such as family predisposition, obesity, diabetes, or pre-existing hypertension.
From a cardiology perspective, the physiological link between PTSD and cardiovascular disease is well substantiated. Chronic activation of the sympathetic nervous system in PTSD leads to sustained surges of catecholamines (epinephrine and norepinephrine), endothelial dysfunction, and heightened vascular tone. Over the years, these maladaptive responses accelerate arterial stiffness and dysregulate circadian blood pressure patterns. In this veteran’s case, documented hypertensive crises temporally coincided with acute PTSD exacerbations, underscoring the causal relationship.
Additionally, the downstream effects of uncontrolled hypertension in this patient, episodic chest tightness, reduced exercise tolerance, fatigue, and erectile dysfunction, are consistent with cardiovascular strain secondary to sustained elevated blood pressure.
Based on the clinical trajectory, objective documentation, and accepted pathophysiology, it is my professional opinion, with a reasonable degree of medical certainty, that this veteran’s hypertension is at least as likely as not (≥50% probability) caused and permanently aggravated by his service-connected PTSD.
Sincerely,
[Physician’s Full Name, MD/DO/PA-C]
[Board Certification, if applicable]
[Specialty, e.g., Internal Medicine/Cardiology]
[License Number]
[Contact Information]
Conclusion
In conclusion, the intricate relationship between hypertension and mental health, especially PTSD, is a critical consideration in the evaluation of veterans’ disability claims. Understanding the various pathways to service connection, the impact of modifiable and non-modifiable risk factors is crucial for veterans navigating the complex landscape of disability benefits. Seeking professional advice from accredited legal professionals and staying informed about relevant research can empower veterans in their pursuit of rightful compensation and healthcare support.
FAQs
Can I get VA disability compensation for high blood pressure secondary to PTSD?
Yes, veterans can claim hypertension (high blood pressure) as a secondary condition to PTSD if medical evidence shows a causal or aggravating link between the two.
How does PTSD lead to hypertension?
PTSD triggers chronic stress responses, inflammation, lifestyle changes, and medication side effects that elevate blood pressure.
What causes high blood pressure post-trauma?
Unresolved trauma can keep the body in a heightened stress state, releasing hormones that raise blood pressure over time.
What is the VA rating for hypertension secondary to PTSD?
VA rates hypertension from 10% to 60% based on blood pressure readings and medication requirements.
What is the medical connection between PTSD and hypertension?
Research shows that veterans with PTSD are significantly more likely to develop hypertension due to prolonged stress and nervous system overactivation.
What VA disabilities are secondary to PTSD?
Common VA conditions secondary to PTSD can include hypertension, heart disease, sleep apnea, gastrointestinal disorders, migraines, and depression or anxiety-related conditions.
What is included in a nexus letter for hypertension secondary to PTSD?
A nexus letter is an independent medical opinion from a qualified provider stating that a veteran’s hypertension is “at least as likely as not” caused or worsened by PTSD.
Also read: Securing VA Disability Rating and Benefits for Hypertension
At Prestige Veteran Medical Consulting, a veteran-owned company, we specialize in Independent Medical Opinions (IMOs) known as Nexus letters.
Our purpose is to empower YOU, the veteran, to take charge of your medical evidence and provide you with valuable educational tools and research to guide you on your journey.
Understanding the unique challenges veterans face, our commitment lies in delivering exceptional service and support.
Leveraging an extensive network of licensed independent medical professionals, all well-versed in the medical professional aspects of the VA claims process, we review the necessary medical evidence to incorporate in our reports related to your VA Disability Claim.
Prestige Veteran Medical Consulting is not a law firm, accredited claims agent, or affiliated with the Veterans Administration or Veterans Services Organizations. However, we are happy to discuss your case with your accredited VA legal professional.