The PTSD Disability Benefits Questionnaire (DBQ) form plays a key role in determining your VA disability rating and ensuring your condition is accurately represented. Completing this standardized form thoroughly helps document how your mental health symptoms impact daily life, work, and relationships, ultimately influencing the benefits you receive.
In this detailed blog, learn what the VA considers during their evaluation and how to approach the PTSD DBQ strategically to achieve the compensation you truly deserve.
Table of Contents
How a PTSD DBQ Strengthens Your VA Disability Case
A Post-Traumatic Stress Disorder (PTSD) Disability Benefits Questionnaire is a standardized VA form that provides objective medical evidence when filing or appealing a veteran’s disability claim. This DBQ form, created by the U.S. Department of Veterans Affairs, ensures that a licensed VA or private mental health provider, such as a psychiatrist or psychologis,t documents a veteran’s PTSD diagnosis, symptoms, and the impact of those symptoms on daily life.
A Disability Benefits Questionnaire not only confirms the diagnosis under DSM-5 criteria but also explains how PTSD affects occupational and social functioning, which directly influences a veteran’s disability rating percentage.
Essential Functions of a PTSD DBQ in a VA Claim:
- Confirms a formal diagnosis in accordance with Diagnostic and Statistical Manual of Mental Disorders (DSM-5) criteria for PTSD.
- Documents symptom severity and frequency using VA-approved medical terminology, aligning with rating standards.
- Provides clinical evidence, including relevant medical findings and psychological testing results that support the diagnosis.
- Strengthens the service connection by clearly linking PTSD to specific in-service stressors such as combat exposure, traumatic events, or fear of hostile military activity.
- Differentiates overlapping conditions like traumatic brain injury (TBI) or depression to isolate the specific impact of PTSD.
- Explains how PTSD affects occupational and social functioning, which is critical for determining whether a veteran qualifies for higher ratings (for example, moving from 50% to 70% or even 100%).
For example, a combat veteran experiencing chronic hypervigilance and sleep disturbances may receive a higher rating when their provider thoroughly completes a PTSD DBQ that describes how these symptoms disrupt employment and family life.
Since this information aligns with the VA’s Schedule for Rating Disabilities (38 CFR), specifically the General Rating Formula for Mental Disorders under 38 CFR §4.130, it helps VA raters assess the full extent of impairment and make faster, more accurate rating decisions.
Who Can Complete the DBQ for PTSD?
The VA accepts DBQs for Post-Traumatic Stress Disorder (PTSD) only from professionals qualified and authorized to diagnose and treat psychiatric conditions. Eligible providers include:
- Board-certified psychiatrists
- Licensed psychologists (Ph.D. or Psy.D.)
- VA-employed mental health providers
- Private practitioners (if the veteran chooses)
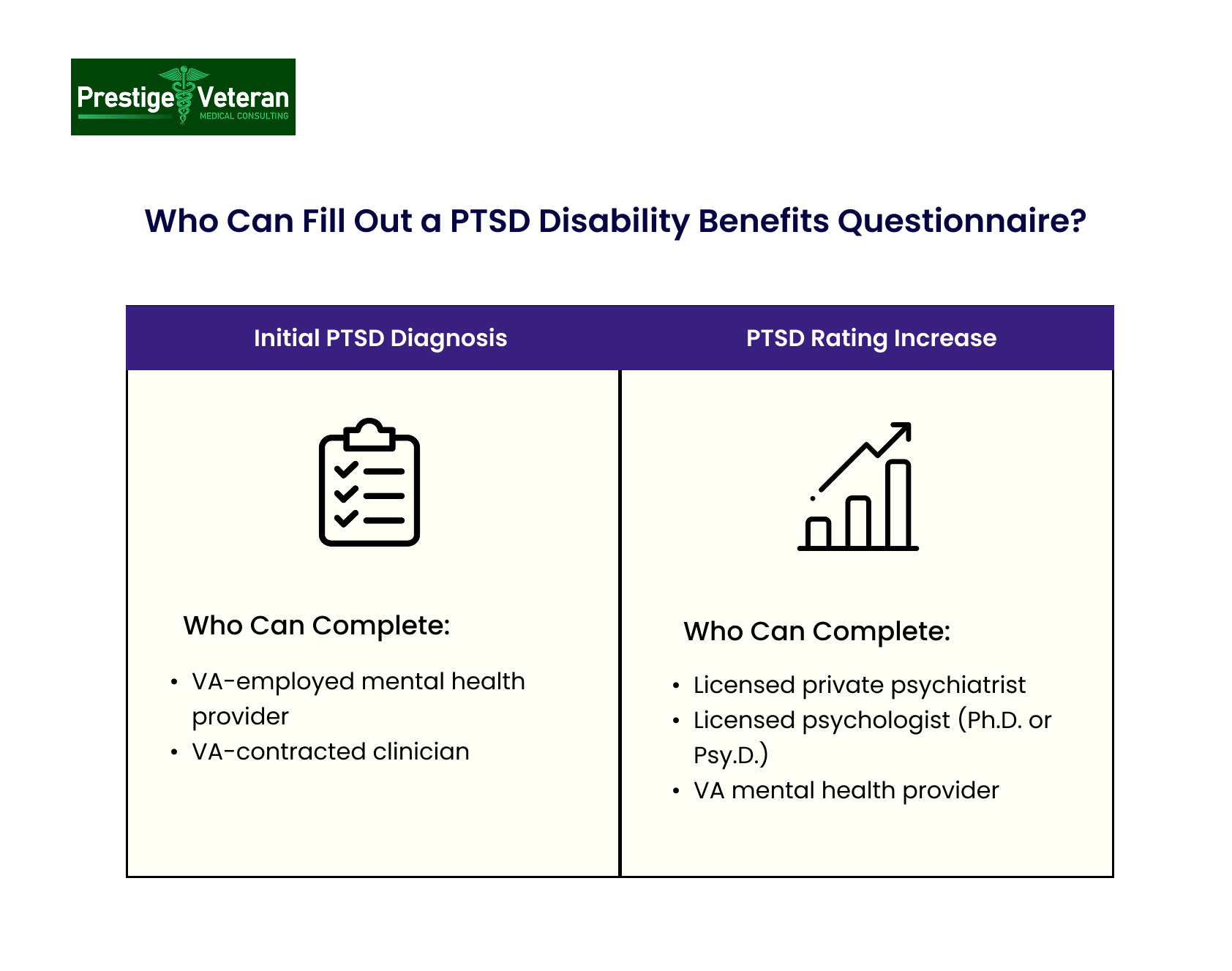
If You’re Filing for an Initial PTSD Diagnosis
When filing a Disability Benefits Questionnaire to establish an initial PTSD diagnosis, generally, a VA-employed or VA-contracted mental health provider may complete the form for service connection purposes. For initial service connection, the VA typically schedules a Compensation and Pension (C&P) examination with one of its clinicians to verify the DSM-5 diagnosis and assess eligibility for benefits.
If You’re Submitting a DBQ for a PTSD Rating Increase
If you already have a confirmed service-connected PTSD diagnosis, a licensed private psychiatrist or psychologist can fill out your DBQ to document current symptoms, functional impairment, and any changes in your condition. This is especially beneficial when seeking an increased VA rating or reevaluation after treatment or due to worsening symptoms. To be valid, the DBQ provider must sign the questionnaire and include their professional credentials.
Who Cannot Complete a PTSD DBQ
The VA does not accept PTSD Disability Benefits Questionnaires from:
- Licensed clinical social workers
- Licensed professional counselors
- Marriage and family therapists
While these professionals may provide treatment, their DBQs are not valid for VA rating purposes.
Explore the full list of VA Disability Benefits Questionnaires.
Understanding the Disability Benefits Questionnaire for PTSD
The Post-Traumatic Stress Disorder (PTSD) Disability Benefits Questionnaire (DBQ) is a standardized VA form used to assess the severity, diagnosis, and functional impact of PTSD in veterans. It ensures that each claim is evaluated according to VA regulatory standards under 38 CFR Part 4. Understanding this form helps veterans to accurately communicate their symptoms to support their disability rating.
I. Diagnostic Summary
This section identifies whether the veteran currently meets the DSM-5 diagnostic criteria for PTSD and lists all mental health conditions with their ICD codes. When multiple diagnoses such as depression, anxiety, or traumatic brain injury (TBI) are present, the examiner must clarify which symptoms are tied to each disorder. Proper differentiation of symptoms is essential for accurate service connection and fair disability evaluation.
II. Occupational and Social Impairment
Here, the examiner evaluates how PTSD affects the veteran’s ability to work, maintain relationships, and manage daily responsibilities. Impairments are rated from mild symptoms with occasional work disruption to total occupational and social impairment, indicating severe dysfunction. Veterans with severe functional limitations may qualify for higher disability percentages and compensation under VA rating criteria.
III. Clinical Findings and Evidence Review
The examiner reviews all relevant evidence, including service treatment records, VA medical documentation, and private healthcare reports. Details about the veteran’s social, marital, educational, and occupational background, as well as any legal or substance-use history, are also documented.
This section of the PTSD DBQ establishes the medical link or nexus between the veteran’s service-related trauma and current psychological condition, as well as shows progression over time.
IV. PTSD Diagnostic Criteria (DSM-5)
This section of the Disability Benefits Questionnaire verifies that the veteran meets the DSM-5 Criteria A–H for a confirmed PTSD diagnosis. These include:
- Criterion A: Exposure to actual or threatened death, serious injury, or sexual violence.
- Criterion B: Intrusive memories, flashbacks, or nightmares.
- Criterion C: Avoidance behaviors related to trauma.
- Criterion D: Negative mood changes and cognitive distortions.
- Criterion E: Arousal symptoms such as hypervigilance or sleep disturbance.
To meet VA requirements, the veteran must show that symptoms persist longer than one month and cause significant distress or functional impairment not attributable to substances or other conditions (Criteria F, G, and H). Each criterion ensures the diagnosis is medically justified and service-connected for a VA rating claim.
V. Symptoms and Behavioral Observations
The PTSD DBQ lists 31 mental health symptoms to evaluate the severity of your condition. Key symptoms relevant to VA evaluations include:
- Chronic sleep disturbance
- Anxiety
- Depression
- Suicidal ideation
- Impaired judgment or concentration
The examiner observes how these symptoms appear during the evaluation to assess the veteran’s mental state and the reliability of self-reporting. These findings are critical in determining the severity of symptoms and the final VA disability rating.
VI. Competency and Remarks
Finally, the examiner determines whether the veteran can manage personal finances independently or requires fiduciary support. Additional notes, psychological test results, and medical opinions by the examiner give a complete summary of the veteran’s overall mental health and functional capacity.
How to Prepare for the PTSD DBQ and C&P Exam
Effectively completing a PTSD DBQ and Compensation & Pension (C&P) exam requires veterans to have a mindset to communicate the full scope of their symptoms.
Here are essential strategies to prepare effectively:
1. Know and Describe Your In-Service Stressor(s)
Be prepared to clearly explain the traumatic event(s) from your military service that triggered your PTSD. Outline the who, what, when, where, and how the incident happened. Use VA Form 21-0781 to document your in-service stressors in writing when applicable. If you discuss personal assault experiences, consider completing VA Form 21-0781a.
For example, if you witnessed a fellow soldier killed by an IED, describe the moment, your emotional response, and how the memory continues to affect you even today.
The VA must validate the existence and severity of the trauma to establish service connection. The more specific and detailed you are, the stronger your case.
2. Bring Supporting Documentation
Supporting documentation often helps the examiner understand the full timeline and severity of your VA PTSD claim. Gather and organize:
- Service treatment records showing mental health complaints during active duty
- Post-service medical records from VA or civilian mental health providers
- Lay statements (VA Form 21-10210) from fellow service members, family, or friends that describe the trauma you experienced and how your symptoms affect your daily life
- Employment records indicating reduced productivity, frequent absences, or job termination
- Current prescriptions or therapy notes documenting your ongoing psychiatric care, such as prescribed antidepressants, or weekly counseling sessions.
3. Be “Uncomfortably Honest” About Your Symptoms
Many veterans underreport symptoms due to embarrassment, pride, or fear of stigma. Avoid this. Be open, even if it feels uncomfortable, about your mental health challenges, including suicidal thoughts, memory issues, or problems with hygiene or aggression.
Example: A veteran once described breaking down in tears while stuck in traffic because the honking reminded him of gunfire. This helped document his occupational and social impairment accurately.
Since the PTSD DBQ and C&P exam are designed to assess the real-life impact of symptoms, downplaying them can increase the risk of receiving a lower rating.
4. Study the VA’s PTSD Rating Criteria and DBQ Format
Familiarize yourself with the PTSD DBQ (Initial) and the VA’s rating criteria before the exam. Understanding how the VA defines impairments such as “difficulty adapting to stressful circumstances” or “impaired impulse control” helps you describe your experiences more precisely.
For example, if hypervigilance makes you avoid crowded places or has led to quitting jobs, mention this directly. Ask your provider to use the exact phrases from §4.130 and to clearly differentiate overlapping conditions.
5. Document Your Daily Functioning in a Journal
Keep a symptom journal for 2–4 weeks before the exam. Record things like insomnia, flashbacks, missed workdays, or emotional outbursts.
For instance, you might record: “April 17, 2025 – Woke up from nightmares, couldn’t focus at work, snapped at a coworker, and ended the day feeling numb and drained.”
Your provider can include this real-world data in the PTSD Disability Benefits Questionnaire to illustrate how your symptoms disrupt your daily life, supporting higher disability ratings (up to 100%) when justified.
6. Talk About Work and Social Functioning
Your VA rating largely depends on how PTSD affects occupational and social functioning. When filling the PTSD DBQ, be specific about challenges such as:
- Frequent absences or difficulty focusing at work
- Avoiding coworkers or authority figures
- Strained relationships with family or friends
- Low motivation or poor hygiene
Tip: Reflect on the last 6–12 months. How has PTSD changed your job performance or personal life?
These details are noteworthy for the VA because they reveal the practical impact of your mental health struggles on your daily life.
7. Bring a Trusted Support Person (If Allowed)
If allowed, bring a spouse, family member, or close friend who witnesses your daily struggles. They can help you stay calm, recall important details, and provide valuable observations of your mood, memory, or behavior. Their perspective can help the examiner better understand the real effects of your PTSD.
Hence, proper preparation for the C&P exam and DBQ ensures that veterans offer the critical evidence needed to support their PTSD claim and obtain a fair VA disability rating.
What Veterans Are Asked During a VA PTSD DBQ Evaluation
When veterans attend a Compensation and Pension (C&P) exam for PTSD, they are asked a series of detailed questions to help the VA understand the severity, frequency, and impact of their symptoms. These questions from the Disability Benefits Questionnaire help to assess how mental health struggles affect the quality of your overall life.
You may be expected to answer questions such as:
- Have you been diagnosed with PTSD according to DSM-5 criteria, and when was the diagnosis made?
- What specific traumatic events during service contributed to your PTSD symptoms?
- When did you first begin experiencing PTSD-related symptoms?
- How do these symptoms impact your ability to work, maintain relationships, or perform daily activities?
- Do you experience recurring nightmares, flashbacks, or intrusive memories?
- How often do you feel anxious, depressed, or emotionally detached?
- What triggers or situations worsen your PTSD symptoms?
- Have personal or family issues contributed to worsening your symptoms?
- Do you experience anger, irritability, or difficulty concentrating?
- Have you ever had thoughts of self-harm or suicidal ideation?
These PTSD DBQ questions help the VA determine the level of disability and ensure veterans receive the support and benefits they deserve.
4 DBQ Mistakes Veterans Should Avoid
Here are some avoidable mistakes in a PTSD DBQ and how they can negatively affect your VA disability claim.
Minimizing or Withholding Symptoms
Some veterans downplay their mental health challenges out of embarrassment or fear of judgment. This often results in a lower disability rating or a denial because the VA lacks full evidence of symptom severity and functional impact.
Incomplete DBQ Forms
If the provider skips sections or fails to list specific PTSD symptoms, the VA may disregard the Disability Benefits Questionnaire form entirely or rely on less favorable evidence. Make sure all boxes are checked and descriptions are detailed.
Confusing PTSD with Other Disorders
PTSD frequently overlaps with depression, anxiety, and other conditions, but each carries a distinct diagnostic code and rating criteria. Failing to distinguish symptoms may lead the VA to misclassify your mental health condition or underestimate symptoms, resulting in a lower VA rating.
Using an Unqualified Examiner
A PTSD Disability Benefits Questionnaire filled by an examiner unfamiliar with VA terminology and rating criteria can weaken your nexus evidence in some cases. Choose a private provider experienced with DBQs and VA standards to ensure accurate medical assessments and form completion.
When Should You File for a PTSD Rating Increase?
If your PTSD symptoms have become more severe since your last VA rating, it may be time to file a VA claim for an increase. That’s where the PTSD Disability Benefits Questionnaire helps the VA understand how your condition has worsened and whether your current rating still reflects your level of impairment.
Signs It Might Be Time to Request a PTSD DBQ Increase
You might consider filing for a higher rating by submitting VA Form 21-526EZ if you’re experiencing:
- Job loss or reduced work hours because of PTSD symptoms
- Growing social withdrawal or strain in personal relationships
- More frequent panic attacks, suicidal thoughts, or a need for hospitalization
- Memory problems or difficulty maintaining personal hygiene
For example, a veteran rated at 30% for PTSD began noticing worsening symptoms such as frequent panic attacks, difficulty concentrating, and withdrawal from family life. Recognizing this decline, the veteran filed a VA claim for an increased rating and submitted a PTSD increase DBQ along with updated medical records, therapy notes, and lay statements.
With this supporting evidence, the VA may raise the veteran’s rating to 50% or higher, reflecting the greater impact on daily functioning.
If You’re in Crisis or Thinking About Suicide
You are not alone. Free, confidential help is available 24/7 through the Veterans Crisis Line:
- Call: 988, then press 1
- Text: 838255
- Chat: VeteransCrisisLine.net/Chat
You do not need to be enrolled in VA benefits to use the Veterans Crisis Line.
Disclaimer: The information in this article is for educational purposes and is not medical, psychological, or legal advice. VA disability outcomes depend on your individual facts and evidence. Always consult a licensed mental-health professional and/or a VA-accredited representative/attorney for advice on your specific case.
Final Thoughts
A well-documented DBQ for Post-Traumatic Stress Disorder can greatly strengthen your VA disability claim by clearly showing how your symptoms impact your life and ability to work. Veterans should ensure their examiner understands VA rating standards, includes specific examples of impairment, and links the diagnosis directly to service-related trauma.
If your PTSD has worsened over time, don’t think twice before updating your Disability Benefits Questionnaire to justify a higher rating. Veterans must remember that seeking help and properly documenting their struggles is a step toward getting the recognition and support they have earned through their military service.
Frequently Asked Questions (FAQs)
What is a DBQ for PTSD for VA?
A Post-Traumatic Stress Disorder (PTSD) Disability Benefits Questionnaire (DBQ) is a standardized VA form used to document a veteran’s PTSD diagnosis, symptomatology, and functional impact.
How to answer the PTSD DBQ questions?
Answer every question honestly and specifically, describing the frequency, severity, and real-life impact of your PTSD symptoms on work, relationships, and daily functioning.
How to prove PTSD for a VA claim?
Submit a VA-verified diagnosis under DSM-5, credible evidence of an in-service stressor, and a medical nexus letter linking the trauma and current PTSD symptoms.
What is the C&P exam for PTSD increase?
It’s a VA evaluation where a licensed examiner reviews your PTSD symptoms and functional decline to determine if your disability rating should be increased.
How to get a 50% VA rating for PTSD?
Show consistent evidence of moderate symptoms like panic attacks, mood instability, and difficulty maintaining work or social relationships, documented in a completed PTSD DBQ.
What to say to get 70% PTSD compensation?
Describe in detail how your PTSD severely limits your ability to work, maintain relationships, and manage daily life, providing honest examples of occupational and social impairment.
What is 70 percent PTSD DBQ?
A 70% PTSD DBQ documents serious mental health symptoms and significant functional impairment that justify a 70% VA disability rating under VA criteria.
How to increase PTSD rating from 70% to 100%?
Provide strong medical and lay evidence through a DBQ showing total occupational and social impairment due to worsening PTSD symptoms.
Also read: Proposed New Rules for PTSD VA Compensation
At Prestige Veteran Medical Consulting, a veteran-owned company, we specialize in Independent Medical Opinions (IMOs) known as Nexus letters.
Our purpose is to empower YOU, the veteran, to take charge of your medical evidence and provide you with valuable educational tools and research to guide you on your journey.
Understanding the unique challenges veterans face, our commitment lies in delivering exceptional service and support.
Leveraging an extensive network of licensed independent medical professionals, all well-versed in the medical professional aspects of the VA claims process, we review the necessary medical evidence to incorporate in our reports related to your VA Disability Claim.
Prestige Veteran Medical Consulting is not a law firm, accredited claims agent, or affiliated with the Veterans Administration or Veterans Services Organizations. However, we are happy to discuss your case with your accredited VA legal professional.













